Review
HJOG 2022, 21 (3), 121-128 | doi: 10.33574/hjog.0508
Kehinde S. Okunade1,2, Adaiah Soibi-Harry2, Tonia Onyeka3, John B. Ogunyemi2, Olufemi Thomas-Ogodo2, Adebola A. Adejimi4, Austin C. Okoro2, Benedetto Osunwusi2, Sunusi R. Garba2, Rose I. Anorlu1,2
1Department of Obstetrics & Gynaecology, College of Medicine, University of Lagos, Surulere, Lagos, Nigeria
2Department of Obstetrics & Gynaecology, Lagos University Teaching Hospital, Surulere, Lagos, Nigeria
3Department of Anaesthesia/Pain & Palliative Care Unit, College of Medicine, University of Nigeria, Ituku-Ozalla Campus, Enugu, Enugu State, Nigeria
4Department of Community Health and Primary Care, College of Medicine, University of Lagos, Surulere, Lagos, Nigeria
Correspondence: Kehinde Sharafadeen Okunade, Department of Obstetrics & Gynaecology, College of Medicine, University of Lagos & Lagos University Teaching Hospital, e-mail: sokunade@unilag.edu.ng
Abstract
Background: The timing of recurrence of epithelial ovarian cancer (EOC) after a standard primary treatment is an important indicator of the degree of response of the tumour to treatment. It, however, remains unclear if the timing of recurrence will predict survival outcomes.
Aim: This study explored the impact of timing of recurrence after an initial response to standard primary treatment on the overall survival (OS) of patients with EOC.
Methods: Data was extracted from the records of patients who underwent standard primary treatment and follow-up after EOC diagnosis between January 2011 and December 2020. The Kaplan-Meier survival estimates and Cox proportional hazards model adjusted for covariates were used for analyses.
Results: The risks of recurrence of EOC increased steadily with increasing time from the start of primary treatment from 13.6% in 6-months to 71.0% after 12-months. In the final multivariate analyses, recurrence within 6 months of treatment was a significant independent predictor of poor OS in EOC patients (hazard ratio=7.23, 95%CI: 3.87–13.51, P<0.01).
Conclusion: Our study suggests that recurrence within 6-months is an important prognostic predictor of poor OS in EOC. Early tumour recurrence may be a useful surrogate of OS and thus this information should be considered in the design of future tailored randomized controlled trials. Future strategies to improve OS in EOC patients should focus on identifying effective measures to prevent early tumour recurrence.
Keywords: Epithelial ovarian cancer, mortality, overall survival, recurrence, surrogate
Introduction
Ovarian cancer is the second most common gynecologic malignancy after cervical cancer in Nigeria.1,2 In 2020, there were 313,959 new cases and 207,252 deaths from ovarian cancer worldwide and by 2040, these numbers are expected to rise by almost 37% to 428,966 new cases and by 50% to 313,617 cancer deaths.3 Up to 90% of ovarian cancer are of epithelial origin (EOC)4–6 with an overall 5-year survival rate of 30–48% despite the standard surgery and chemotherapy treatment.7 To improve overall survival (OS) in EOC, it is important to provide personalized care such as the institution of more intensive and individualized follow-up surveillance plans8 to women who responded to the standard primary treatment with surgery and platinum-based chemotherapy.7 Therefore, it is extremely valuable to design a risk-stratification approach based on certain patient and tumour characteristics to identify the major predictors of the gold-standard survival endpoint (OS) in patients with EOC.9
The outcome of EOC patients is generally poor after recurrences, with a low response to subsequent chemotherapy and/or surgery and an estimated median survival of that is less than 12 months.10 However, this is unpredictable and can vary from study to study.8,10,11 Over 70% of patients managed for EOC will experience recurrence within 2 years and about two-thirds of these will occur within 12-months of treatment.12 Timing of recurrence of EOC after an initial remission is an important indicator of the degree of response of the tumour to treatment,12 however, it remains unclear if the timing of recurrence will predict survival outcomes. It, therefore, becomes imperative to conduct research that will examine and control for the influence of possible confounding factors on the relationship between the timing of tumour recurrence and OS in EOC patients. To bridge this important knowledge gap, our current study, analysed a cohort of EOC patients managed over 10 years in a gynecologic oncology unit of a tertiary hospital in Lagos, Nigeria to determine the impact of timing of recurrence after a period of remission of on the OS of these patients.
Materials and Methods
Study design and settings
This was a retrospective cohort study of 176 patients diagnosed with EOC and who had standard primary treatment followed by at least 3-years of follow-up between January 2011 and December 2020 at the gynecologic oncology unit of a university teaching hospital. The teaching hospital is a multi-specialities referral centre that provides services to over 25 million residents of Lagos and parts of its surrounding States of Ogun and Oyo in Southwest Nigeria.
Study population
Data of the 176 women who met the eligibility criteria were retrieved from the in-patient register and medical case records in the gynecologic oncology unit of the hospital. Criteria for inclusion of women in the study were: 1) confirmation of EOC by histopathology, 2) completion of a full course of standard primary treatment consisting of either primary debulking surgery (PDS) and postoperative adjuvant chemotherapy (ACT) or preoperative neoadjuvant chemotherapy (NACT), interval debulking surgery (IDS), and postoperative adjuvant chemotherapy (ACT), 3) patients with complete medical records and laboratory test results required for data analyses. We excluded women who: 1) failed to complete the standard primary treatment, and 2) had severe postoperative complications that required prolonged admission in the high-dependency or intensive-care unit.
Participants’ recruitment and data collection
Relevant data of eligible women such as age, menopausal status, parity, pre-existing medical comorbidity (including diabetes mellitus, hypertension, liver, and kidney disorders), body mass index (BMI) defined as body weight in kilograms divided by the square of height in meters, serum cancer antigen 125 (CA-125) levels, International Federation of Gynecology and Obstetrics (FIGO) stage of the disease, presence of ascites and histologic subtype of the tumour were collected using a proforma designed for the study. The mortality data were collected after 3 years of treatment completion until December 2020.
Definition of important variables and study endpoint
In this study, we defined standard primary treatment as a full course of treatment consisting of either PDS and 6-cycles of platinum-based postoperative ACT administered intravenously every 3 weeks or IDS in-between 3 to 4 cycles each of platinum-based preoperative NACT and postoperative ACT administered intravenously every 3 weeks.7 Tumour recurrence was the presence of any clinical or radiological evidence of the disease after an initial response to the standard primary treatment. A detectable disease was defined as the clinical evidence of a tumour on pelvic examination; and/or the radiological presence of a new pelvic tumour on abdominopelvic USS or CT scan with or without abnormal (>35 IU/ml) or increasing serum CA-125 levels.12 The study endpoint, overall survival (OS), was defined as the length of the time from the start of primary treatment that the patients diagnosed with EOC were still alive.8,9 The OS data were censored after a 3-year follow-up until December 2020.
Statistical analysis
SPSS statistical computing software version 27 (IBM Corp., Armonk, NY, USA) for Windows was used for data analyses. Patients’ sociodemographic and clinical characteristics were computed using descriptive statistics. Categorical variables were presented as frequencies and percentages while continuous variables were presented as mean (± standard deviation) if normally distributed or median (interquartile range) if skewed. The mean or median values of age, BMI and serum CA-125 levels were used as the stratifying cut-off values in the univariate and multivariate analyses. Kaplan-Meier analysis was performed to estimate the OS after recurrence and the group difference in survival function was compared using the Log-rank (Cox-Mantel) test. The hazard ratios (HRs) of death at a 95% confidence interval (CI) were estimated for all patients’ characteristics in a predictive model using the Cox proportional hazards analyses to adjust for covariates. The adjusted multivariate models included age and other variables with P<0.20. P <0.05 was reported as statistically significant.
Ethical considerations
Ethics approval was obtained from the hospital’s Ethics Committee (ADM/DCST/HREC/1912) before commencing patients’ medical records retrieval and data collection. Strict adherence to the confidentiality of collected information was ensured throughout the study and reporting of findings.
Results
We retrieved the data of 203 patients who were diagnosed and treated for EOC during the 10-year review period, however, we collated and analysed the data of 176 patients who met the eligibility criteria [Figure 1].
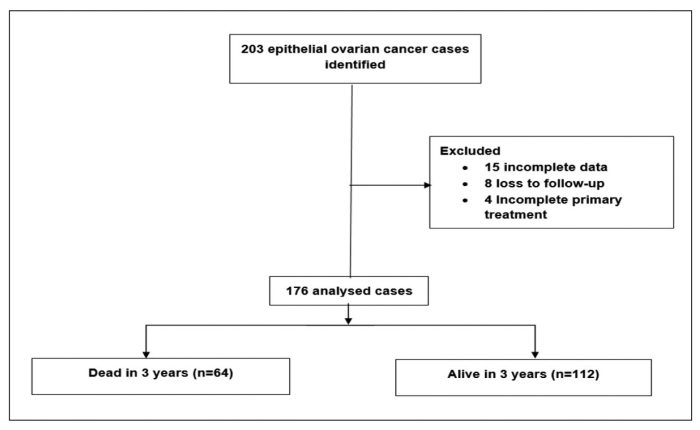 Figure 1. Study flow chart.
Figure 1. Study flow chart.
As shown in Table 1, the risks of recurrence of EOC increased steadily with increasing time from completion of primary treatment from 13.6% in 6-months to 71.0% after 12-months. We also recorded a 3-year mortality risk of 36.4% in the EOC patients. The patients’ mean age and BMI were 50.6 (± 13.2) years and 24.8 (± 5.1) kg/m2 respectively while the median serum CA-125 was 340 (74–1004) U/mL. Most of the patients were multiparous (64.8%, n=114), had co-existing medical morbidity (80.1%, n=141), had PDS as upfront primary treatment (59.1%, n=104), had no ascites (55.7%, n=98), had advanced FIGO stage 3 & 4 diseases (71.6%, 126), and type II histology subtype of tumour (64.2%, n=113). About half of the patients were postmenopausal (n=89, 50.6%) and had optimal debulking surgery (49.4%, n=87).
Using a Kaplan-Meier estimate that stratified the patients into two groups based on their timing of tumour recurrence [Figure 2], recurrence within 6 months of completion of primary treatment had a statistically significant association with OS (P<0.01). In addition, based on a predefined value of P<0.20 as shown in Table 2, parity (P=0.16), menopausal status (P=0.17), BMI (P=0.02), type of upfront primary treatment (P=0.17), ascites (P=0.01), FIGO stage (P=0.03), and surgical debulking status (P=0.10) were associated with OS. However, following adjustments for these covariates in the final multivariate analysis, recurrence within 6 months of treatment was recorded as a significant independent predictor of poor OS in EOC patients (HR=7.23, 95%CI: 3.87–13.51, P<0.01) [Table 3].
 Figure 2. Kaplan-Meier curve showing overall survival stratified by timing of recurrence in women with epithelial ovarian cancer (P<0.01).
Figure 2. Kaplan-Meier curve showing overall survival stratified by timing of recurrence in women with epithelial ovarian cancer (P<0.01).
Discussion
Epithelial ovarian cancer is the most lethal gynecologic cancer13 due to its late diagnosis and frequent recurrences.12,14 Early recurrence of epithelial ovarian cancer (EOC) is relatively uncommon and therefore, reports on the outcomes of this group of patients are limited. Although it is well recognized that the prognosis is poor for women with recurrent disease, it remains unclear if the timing of recurrence will predict survival outcomes. Our study found a 6-month recurrence and mortality risks of 13.6% and 36.4%, respectively. Only early recurrence was recorded on multivariate analysis as an independent prognostic predictor of poorer OS.
OS in patients with EOC has been associated with various patients’ specific clinical and tumour characteristics.15,16 However, only a few studies have examined the direct impact of timing of recurrence on the survival of EOC patients,17 and consistent with previous findings, our study confirmed tumour recurrence within 6-months as an important independent predictor of OS in patients with EOC. Women who had treatment for EOC are generally at risk of having recurrences at some point after remission12,18 with over half of these occurring within 12-months of treatment.12 However, there are worldwide variations in the rates of recurrence in EOC18–20 but the patterns of mortality remain almost similar despite standard treatment with surgery and chemotherapy.8,21,22 This may be explained by the predominantly late presentation of patients due to the insidious nature of the disease and its non-specific symptoms which may mimic other conditions23,24 such as abdominal swelling or bloating, pelvic or abdominal pain, unexplained weight loss, changes in bowel habits, early satiety or loss of appetite, and increased urinary frequency or urgency.23
The study may be limited by the 3-year follow-up period adopted for mortality assessment which may be too short, and thus may account for the relatively high OS recorded. Secondly, this is also a single institutional study in an urban setting, and thus, the findings may not be generalized to other institutions especially those in rural locations. Lastly, the study did not capture or control for the possible effects of any additional or secondary treatment received by patients after the diagnosis of recurrence on the study endpoint, OS. However, these patients underwent primary surgery and staging by gynecologic oncologists in a multi-disciplinary team setting. In addition, a central pathology review by expert gynecologic oncology pathologists was used in the analysis of the surgical specimens obtained during the period under review.
Conclusion
Our findings suggest that recurrence within 6-months is an important prognostic factor that predicts poor OS in EOC. Early tumour recurrence may thus be a useful surrogate of OS and thus this information should be considered in the design of future tailored randomized controlled trials. Furthermore, as recurrent EOC is not a curative disease, future strategies to improve OS in EOC patients should focus on identifying effective measures to prevent early tumour recurrence.
Acknowledgements
We appreciate the invaluable assistance of the staff of the gynecologic oncology division of the hospital’s medical records department without whom access to the patients’ medical records would not have been possible. We also acknowledge the immense contribution to the data retrieval and collation by resident doctors in the oncology and pathological studies unit of the obstetrics and gynaecology department.
Declaration of Conflicting Interests
The authors have no conflicts of interest.
Funding
This study was conducted through the protected time support provided by the Fogarty International Center of the National Institutes of Health under Award Numbers D43TW010134, D43TW010543 and D43TW010934. The views expressed by the authors are theirs alone and do not reflect the official views of the National Institutes of Health.
References
1. Yakasai IA, Ugwa EA and Otubu J. Gynecological malignancies in Aminu Kano Teaching Hospital Kano: A 3-year review. Niger J Clin Pract. 2013;16(1):63-66.
2. Ugwu EO, Iferikigwe ES, Okeke TC, et al. Pattern of gynaecological cancers in University of Nigeria Teaching Hospital, Enugu, South-eastern Nigeria. Niger J Med. 2011;20(2):266-269.
3. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249.
4. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
5. Siegel RL, Miller KD and Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30.
6. National Cancer Institute. SEER Survival Monograph Cancer Survival Among Adults: U.S. SEER Program, 1988-2001 Patient and Tumor Characteristics.; 1988. http://seer.cancer.gov/publications/survival. (1988, accessed 26 April 2022).
7. Matulonis UA, Sood AK, Fallowfield L, et al. Ovarian cancer. Nat Rev Dis Primers. 2016;2:16061.
8. Okunade KS, Adejimi AA, Ohazurike EO, et al. Predictors of Survival Outcomes After Primary Treatment of Epithelial Ovarian Cancer in Lagos, Nigeria. JCO Glob Oncol. 2021;7:89-98.
9. Driscoll JJ, Rixe O. Overall survival: still the gold standard: why overall survival remains the definitive endpoint in cancer clinical trials. Cancer J. 15(5):401-405.
10. Davis A, Tinker A v and Friedlander M. “Platinum resistant” ovarian cancer: what is it, who to treat and how to measure benefit? Gynecol Oncol. 2014;133(3):624-631.
11. John-Olabode SO, Okunade KS, Olorunfemi G, et al. Pretreatment Neutrophil-to-Lymphocyte Ratio: A Prognostic Biomarker of Survival in Patients With Epithelial Ovarian Cancer. Cureus. 2021;13(7):e16429.
12. Okunade KS, Adetuyi IE, Adenekan M, et al. Risk predictors of early recurrence in women with epithelial ovarian cancer in Lagos, Nigeria. Pan Afr Med J. 2020;36:272.
13. Craveiro V, Yang-Hartwich Y, Holmberg JC, et al. Phenotypic modifications in ovarian cancer stem cells following Paclitaxel treatment. Cancer Med. 2013;2(6):751-762.
14. Guérin S, Doyon F and Hill C. The frequency of cancer in France in 2006, mortality trends since 1950, incidence trends since 1980 and analysis of the discrepancies between these trends. Bull Cancer. 2009;96(1):51-57.
15. Liu XH, Man YN and Wu XZ. Recurrence season impacts the survival of epithelial ovarian cancer patients. Asian Pac J Cancer Prev. 2014;15(4):1627-1632.
16. Chan JK, Tian C, Monk BJ, et al. Prognostic factors for high-risk early-stage epithelial ovarian cancer. Cancer. 2008;112(10):2202-2210.
17. Chan JK, Tian C, Teoh D, et al. Survival after recurrence in early-stage high-risk epithelial ovarian cancer: a Gynecologic Oncology Group study. Gynecol Oncol. 2010;116(3):307-311.
18. Amate P, Huchon C, Dessapt AL, et al. Ovarian Cancer: Sites of Recurrence. International Journal of Gynecologic Cancer. 2013;23(9):1590-1596.
19. Yang ZJ, Zhao BB and Li L. The significance of the change pattern of serum CA125 level for judging prognosis and diagnosing recurrences of epithelial ovarian cancer. J Ovarian Res. 2016;9(1):57.
20. Armstrong DK, Bundy B, Wenzel L, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354(1):34-43.
21. Winter WE, Maxwell GL, Tian C, et al. Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007;25(24):3621-3627.
22. Okunade K, Dawodu O, Adenekan M, et al. Prognostic impact of pretreatment thrombocytosis in epithelial ovarian cancer. Niger J ClinPract 2020;23:1141-7.
23. Sundar S, Neal RD and Kehoe S. Diagnosis of ovarian cancer. BMJ 2015;351:h4443
24. Okunade K, Okunola H, Okunowo A, et al. A five year review of ovarian cancer at a tertiary institution in Lagos, South-West, Nigeria. Niger J Gen Pract 2016;14:23-7.