Research
HJOG 2023, 22 (2), 63-75 | doi: 10.33574/hjog.0526
Olha Proshchenko1, Iryna Ventskivska1, Serhii Vasyliuk2, Artem Mykytiuk3
1Bogomolets National Medical University, Kyiv, Ukraine
2Ivano-Frankivsk National Medical University, Ivano-Frankivsk, Ukraine
3Vasyl Stefanyk Precarpathian National University, Ivano-Frankivsk, Ukraine
Correspondence: Serhii Vasyliuk MD, PhD, Professor, Department of Traumatology, Orthopaedics and Emergency Military Surgery, Ivano-Frankivsk National Medical University, Ivano-Frankivsk, Ukraine, Tel.: +38 067 804 19 74, e-mail: surifnmu@gmail.com
Abstract
Background and aims. The principles of enhanced recovery in operative gynecology, comorbidity, and a multimodal approach in perioperative support require comprehensive study and optimization, and the ambiguity of literature reports determines the relevance of this study. The aim of this study was to evaluate the parameters of perioperative monitoring after hysterectomy for uterine leiomyoma in patients of reproductive age using enhanced recovery after surgery protocols and their impact on quality of life indicators.
Materials and methods. To evaluate the effectiveness of the enhanced recovery protocol after hysterectomy, two groups were formed: the main prospective group, which included 46 patients, who underwent vaginal hysterectomy without appendages and 36 patients with abdominal hysterectomy, who used enhanced recovery after surgery (ERAS) protocols. The comparison group (group of standard management) included 44 patients who underwent vaginal hysterectomy without appendages and 34 patients with abdominal hysterectomy. The main parameters of monitoring were the postoperative pain level, intraoperative blood loss, diuresis rate, the timing of urinary catheter removal and recovery of peristalsis, as well as individual activation of motor activity.
Results. When using the principles of ERAS, the quantitative assessment of pain level (“absence of pain”) was 1.6 times more severe compared to the data of the comparison group; the timing of urinary catheter removal was 2.0 times shorter, drain removal – 2.7 times shorter, recovery of peristalsis – 1.9 times shorter and individual activation of motor activity – 2.9 times earlier than in patients of the comparison group.
Conclusions. Studies have demonstrated the feasibility of using laparoscopic technology in combination with the ERAS, which demonstrates a fall in the volume of intraoperative blood loss, a decrease in blood and fluid balance, a shortening of the time of invasive intravascular intervention, allows to improve the course of the early postoperative period, relieve postoperative pain syndrome, reduce the risk of intestinal paresis, shorten the rehabilitation period, and, as a result, improve quality of life indicators.
Keywords: Hysterectomy, enhanced recovery after surgery, ERAS, pain level, quality of life indicators
Background and aims
ERAS or “fast-track surgery” (FTS) is a concept that involves a set of measures in the perioperative period aimed at reducing the length of hospitalization and recovery after planned surgical interventions.1-4 Each of these measures individually (according to the principles of evidence-based medicine) affects the recovery process, and the concept of ERAS provides for their integrated use, requires the cooperation of all members of the surgical team, and the data of the ERAS use demonstrate success when several components of the ERAS pathway are implemented together. Successful implementation of the ERAS pathway across the spectrum of gynecological care has the potential to improve patient care and healthcare delivery systems.1,5-7 The application of laparoscopic technologies, but in combination with preoperative preparation and changes in approaches to the management of the postoperative period corresponds to the principles of “fast-track surgery” as much as possible. The concept of “fast track” covers all phases of perioperative treatment: preoperative, intraoperative, and postoperative ones, and involves not only shortening the duration of inpatient treatment, but also potentiation of all components of the treatment process, normalization of vital body functions and quality of life indicators, minimization of the consequences of surgical trauma.1,5-8
As evidenced by the reviewed literature, enhanced recovery after surgery (ERAS) is a multimodal, interdisciplinary approach to optimize patient outcomes by minimizing surgical stress in order to return to normal physiological function.1,5,6 The use of minimally invasive surgery, as a superior method of gynecological surgery, is an integral component of ERAS and is closely related to better postoperative outcomes. Implementation of ERAS programs in minimally invasive gynecologic surgery results in significantly improved clinical outcomes with higher same-day discharge rates, reduced postoperative nausea and vomiting, improved patient satisfaction, and decreased opioid consumption without increasing complications, readmissions, or healthcare costs.5 Although differences between published protocols highlight the need for standardization, the existing literature supports the adoption of ERAS as safe and effective when planning minimally invasive gynecologic surgery (MIGS), and the use of ERAS in MIGS with bowel surgery results in shorter hospital stays, stable postoperative morbidity, and a smaller number of repeated hospitalizations.6
Enhanced recovery after surgery protocols in operative gynecology are currently implemented in many medical institutions, where preference is given to minimally invasive approaches and optimization of the practice of preoperative preparation and standardization of perioperative care, taking into account the principles of the concept of FTS (“fast track”), which allows to personalize rehabilitation measures, improve compliance to treatment options, ensures quick recovery, reduces the time of temporary incapacity and normalizes quality of life indicators.5-8 According to literary sources, the FTS program involves informing and teaching the patient through counseling, which allows to reduce the stress load, metabolic and functional disorders initiated by it, prolonging the treatment: a detailed explanation of all the stages of the perioperative period, proving the need for the patient’s active participation in the recovery process (breathing exercises, early nutrition and activation of daily life), the planned time of stay in the hospital, refusal of bowel preparation and fasting (standard tactics recommended by the European Society of Anesthesiologists, i.e. cessation of solid food intake 6 hours and liquids 2 hours before surgery), reducing the invasion and opioid burden.5-6 Analytical processing of a number of meta-analyses demonstrated a reduction in the length of hospitalization after “major” abdominal surgeries.7
The principles of enhanced recovery in operative gynecology, comorbidity, and multimodal approach in perioperative support require comprehensive study and optimization, and the ambiguity of literature reports determines the relevance of this study.
The aim of this study was to evaluate the parameters of perioperative monitoring after hysterectomy for uterine leiomyoma in patients of reproductive age using enhanced recovery after surgery protocols and their impact on quality of life indicators.
Materials and methods
To evaluate the effectiveness of optimized perioperative measures and postoperative recovery, two groups were formed: the main prospective group (with ERAS) which included 46 patients who underwent vaginal hysterectomy without appendages and 36 patients with abdominal hysterectomy who used enhanced recovery after surgery protocols. The comparison group (without ERAS) included 44 patients who underwent vaginal hysterectomy without appendages and 34 patients with abdominal hysterectomy (Fig. 1). The patients were examined on an outpatient basis, which corresponds to the protocol of enhanced perioperative management and is aimed at reducing perioperative stress and risk of nosocomial infections. Hysterectomy with laparoscopic support in both groups was performed under combined general anesthesia with mechanical ventilation.

Figure 1. Groups of patients selected for evaluation of the effectiveness of optimized perioperative measures and postoperative recovery.
The main monitoring parameters were the level of intraoperative blood loss, diuresis rate, the timing of urinary catheter removal and recovery of peristalsis, as well as individual activation of motor activity. One of the important principles of enhanced recovery is early mobilization, which is impossible without adequate analgesia. The level of postoperative pain was determined using a 100-mm visual analog scale (VAS), where pain levels are represented by the following parameters: 0–4 mm (no pain), 5–34 mm (minor pain), 35–74 mm (moderate pain), 75-100 mm (severe pain). The obtained results made it possible to distinguish statistically significant differences in subjective pain sensation after 6-12 and 24 hours. Satisfaction with the surgical experience was assessed using a telephone questionnaire on the day after discharge and 12 months after surgery. Quality of life indicators was assessed by analytical processing of the MOS SF-36 questionnaire data.
The obtained results were analyzed applying the methods of variation statistics using the average value, standard error, where statistically significant reliability was accepted on the indicator p<0.05. Groups were compared using χ2, Studen’s t-test and odd ratio (OR), we set the confidence interval (CI) at 95%, and we defined it as ±1.96 standard errors.
Results
Preoperative examination requires assessment of risk factors (BMI>40 kg/m2, hypertensive disorders, endocrinopathies, risk of pulmonary embolism and patient’s age, respiratory tract condition, and cardiovascular status). There were no statistically significant differences in body mass index, age and comorbid pathology. The average age of patients in the main group was 45.9±1.3 years, in the comparison group – 46.2±1.6 years, in the control group – 45.7±1.3 years. The structure of indications for surgical intervention in patients with uterine leiomyoma because of which hysterectomy with opportunistic tubectomy without ovaries was performed, in the main and comparative groups is presented in Table 1.
The main laboratory indicators 24 hours after the operation are presented in Table 2. Characterizing the main laboratory indicators, it should be noted that the concentration of platelets and total protein remained at the level of reference physiological values in the group of patients where the principles of the FTS concept were used, while in the comparison group with traditional management of the perioperative period, anemia, hypoproteinemia, and increased glucose levels were noted, which creates prerequisites for disruption of the reparative processes of the wound surface, a subjective feeling of insufficient recovery of strength, and have negative changes in the indicators of quality of life.
As shown in Table 2, a smaller volume of intraoperative blood loss by 25.0% compared to the data of the comparison group (p<0.05) was noted in the main group; the diuresis indicator probably did not differ; in the group with FTS, the intraoperative blood and fluid balance was 1, 9 times lower than in the comparison group.
There is no doubt that the volume of infusion therapy plays an important role in the normalization of the function of the cardiovascular system. As the literature shows, reducing the volume of infusion therapy during surgery from 40 to 15 ml/kg allows avoiding a number of complications concerning the respiratory and cardiovascular systems, speeding up postoperative recovery, and reducing the length of hospitalization.9-10
Adequate anesthesia is the key to reducing the rate of postoperative complications. According to the meta-analysis of A. Rodgers et al., it was concluded that the use of epidural anesthesia reduces mortality, the share of hospital-acquired pneumonia, thrombosis, and thromboembolic complications.11,12 Therefore, adequate analgesia remains one of the components of patient-oriented therapy at the perioperative stage and is important not only from a medical point of view; it is also the prevention of polypharmacy of analgesics and side effects of this group while maintaining the patient’s normal well-being, which required determination of the pain level in the postoperative period.
In the main group, the quantitative assessment of the level of pain (“no pain”) when using FTS principles (41.5% of observations) was more significant (by 1.6 times compared to the data of the comparison group, p˂0.05), i.e., subjective pain sensations in the postoperative period were perceived by the patients of the main group as “severe pain” almost 1.8 times less (19.5% vs. 34.6%), which is a confirmation of the improvement of the postoperative condition during the first day. After 24 hours, pain with the rating of “severe pain” did not differ significantly between groups; however, the category “no pain” was noted 1.9 times more often by patients of the main group.
The data demonstrate the following advantages of the FTS technique (Fig. 2): parameters such as the timing of urinary catheter removal were 2.0 times shorter (that is, more than 14 hours), removal of drains – 2.7 times shorter. It allows to offer early activation of the postoperative period which means reducing the probability of the risk of inflammatory and thromboembolic complications, perioperative respiratory disorders and contribute to the improvement of quality of life indicators.
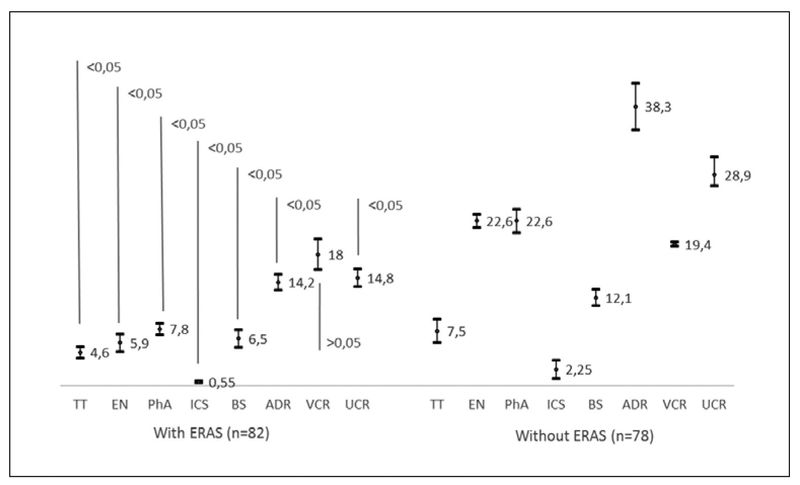
Figure 2. Average terms of medical manipulations and physical recovery of patients after the procedures: TT – treatment time (days); EN – enteral nutrition (h); PhA – physical activity (h); ICS – intensive care stay (h); BS – bowel sounds (h); ADR – abdominal drain removal (h); VCR – venous catheter removal (h); UCR – urinary catheter removal (h).
The final indicator of rational perioperative management are data on recovery of peristalsis (by 1.9 times earlier) and individual activation of motor activity (by 2.9 times earlier than in patients of the comparison group, (р ˂0.05). Individual assessment of patients in the main group revealed their willingness to activate when using FTS already 7 hours after the operation.
In order to prevent thrombosis, a variable pneumocompression system was used intraoperatively which allows to increase blood flow in the vascular bed of the lower extremities, low molecular weight heparins and compression knitwear. Attention was paid to the use of diosmins, which normalize the function of the venous wall and improve lymphatic drainage which is often disturbed in women with uterine fibroids, prolapse of pelvic organs and adhesive disease. These drugs were also included in the program of enhanced recovery after surgery for patients with varicose veins of the lower extremities and chronic pelvic pain syndrome.
A multimodal approach and the implementation of perioperative anesthetic management based on the principles of enhanced recovery when performing hysterectomy in patients of reproductive age made it possible to significantly reduce the length of stay in the hospital, start enteral nutrition and the first liquid intake on the first postoperative day, and perform these surgical interventions before the concept of “one-day” surgery.
The specified optimized approach made it possible to evaluate the following positive aspects: minimal invasiveness, low risk of infectious complications, short courses of antibiotic therapy, mild postoperative pain, cosmetic effect, short hospitalization periods and quick recovery.
As shown in Fig. 3-5, according to the analysis of the MOS SF-36 questionnaires, in the monitoring dynamics of the postoperative period, high indicators were observed in patients who underwent transvaginal hysterectomy associated with laparoscopy, on all scales – PhF, PhRF, BP, V, SRF, ERF and MH which indicates the preservation of a high level of quality of life. It should be noted that the PhF index in the case of transvaginal hysterectomy associated with laparoscopy was significantly higher (on average by 26 points) than in patients with abdominal hysterectomy. PhRF indicators in the groups did not differ statistically and were low, which is typical for this type of surgical intervention. In general, an increase in the physical component of health was noted in the main group by an average of 48.9±1.8 points; in the comparison group – by 36.9±1.6 points compared to the indicators before the surgery.
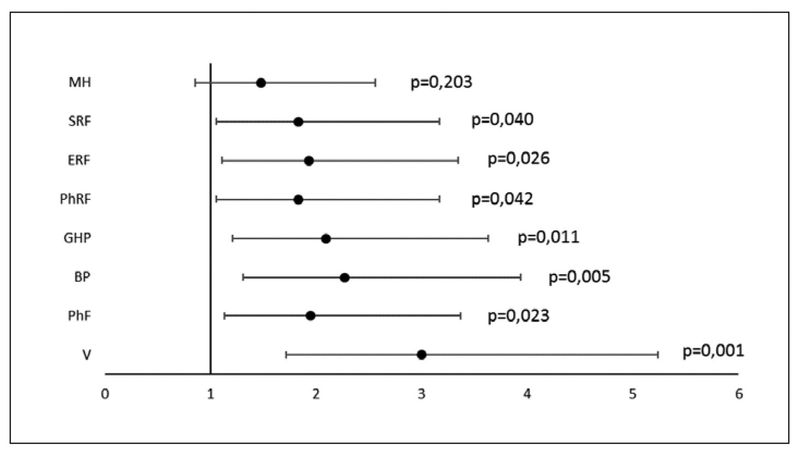
Figure 3. Forest plot of odds ratio (CI 95 %) for quality of life indicators 7 days after hysterectomy in patients with ERAS (n=82): V – vitality; PhF – phisical functioning; BP – bodily pain; GHP – general health perception; PhRF – physical role functioning; ERF – emotional role functioning; SRF – social role functioning; MH – mental health.
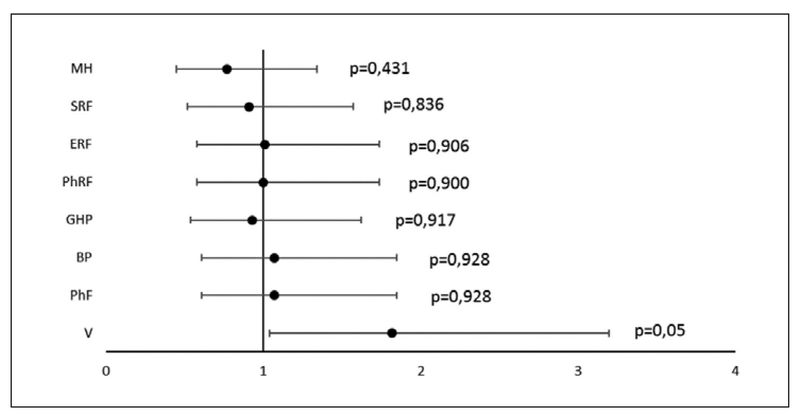
Figure 4. Forest plot of odds ratio (CI 95 %) for quality of life indicators 7 days after hysterectomy in patients without ERAS (n=78): V – vitality; PhF – phisical functioning; BP – bodily pain; GHP – general health perception; PhRF – physical role functioning; ERF – emotional role functioning; SRF – social role functioning; MH – mental health.
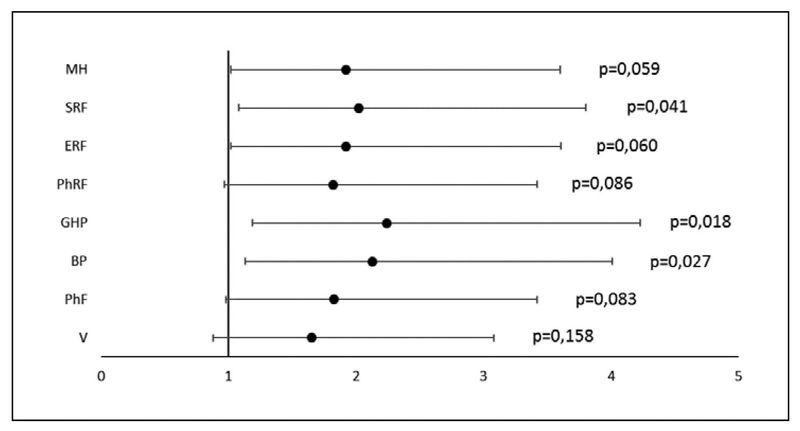
Figure 5. Forest plot of odds ratio (CI 95 %) for quality of life indicators 7 days after hysterectomy in patients with ERAS and without ERAS: V – vitality; PhF – phisical functioning; BP – bodily pain; GHP – general health perception; PhRF – physical role functioning; ERF – emotional role functioning; SRF – social role functioning; MH – mental health.
Testing showed that patients with uterine leiomyoma have problems with the psychological component of health before surgery. They have significantly limited indicators of V, SRF, SRF due to the emotional state and features of mental health, which are characterized by anxiety and depression in comparison with control data. After surgical treatment, when evaluating the mentioned indicators during the hospital stay and characterizing the mental component of health, a tendency to improvement was noted in comparison with the indicators before the procedure. In the main mass of respondents (114 people – 71.3%), the vitality index (V) was quite significant (70.8±2.8 points), which is the evidence of the absence or low fatigue of patients and indicates strong vitality, only 46 (28.7%) patients demonstrated a satisfactory vitality (56.1±2.1 points). In the majority of patients (117-73.1%), the indicator of social functioning in the postoperative period amounted to more than 70 points, which proved a total or partial absence of restriction of social contacts, a normal level of communication; and only 21 (26.9%) patients in the comparison group (without ERAS) had satisfactory social functioning (50 points or less).
The indicator of role functioning in the majority of patients (116 – 72.5%) was due to a good emotional state, in 44 patients (56.4%) in the comparison group (without ERAS) the results obtained were interpreted as a limitation of the performance of everyday activities, due to insufficiently satisfactory emotional condition. The average indicators of mental health (MH) in 132 (82.5%) respondents indicated the absence of anxiety and depressive experiences, and 28 (35.9%) patients of the comparison group (without ERAS) had a moderate anxiety and decrease in positive emotions.
The evaluation of the questionnaire data allowed one year after hysterectomy in 62 cases (38.8%) to establish the full effectiveness of surgical recovery and improvement in the quality of life; in 98 cases (61.3%) – improvement but dissatisfaction with the quality of life due to the following causes was noted: in 13 (13.3%) – due to pelvic floor weakness or apical prolapse, in 34 (34.7%) – due to urinary disorders, in 14 (14.3%) – due to sexual dysfunction (Fig. 6).
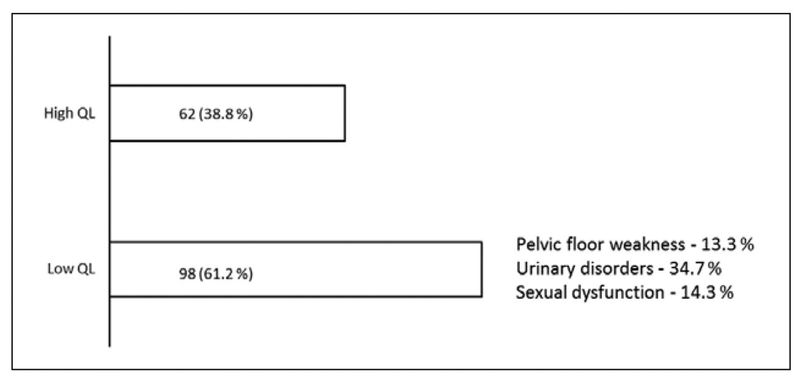
Figure 6. Rehabilitation and quality of life of patients 12 months after the procedure.
The analysis of the obtained results allows to single out transvaginal hysterectomy with laparoscopic assistance as the surgical technique of choice in patients of reproductive age and as the most effective in terms of quality of life indicators when fulfilling all the criteria for selecting patients before its use and depending on the index of somatic health or the performance of simultaneous operations.
Discussion
Improved outcomes and patient satisfaction associated with better postoperative recovery are increasingly replacing traditional perioperative anesthesia care. Rapid surgical approaches have been extensively tested in hysterectomy patients, but the impact on fertility-preserving laparoscopic gynecological surgery, particularly in the treatment of chronic pain, has not been adequately studied.13,14
The recommended treatment for uterine leiomyoma is surgery, but it still has fallings such as postoperative complications and slow recovery. The protocol of enhanced recovery after surgery (ERAS) allows to reduce traumatic stress and promote rapid postoperative recovery of patients, but there are some contradictions regarding the results of different studies. Application of the ERAS protocol after gynecological laparoscopic myomectomy made it possible to reduce the time of the first defecation, the first getting out of bed, stay in the hospital and reduce the frequency of repeated hospitalizations, as well as the frequency of postoperative complications without additional costs.15
Peters A. et al. presented the results of a scientific search for the course of the postoperative period in 410 women with better recovery after surgery.16 In the improved postoperative recovery cohort, there were a 19-minute shorter post-anesthesia care unit stay (P = 0.036), a reduction in postoperative pain and nausea/vomiting (57% reduction in post-anesthesia care unit antiemetics (P < 0.001), a reduction in total narcotic drug use in the perioperative period by 64% (P < 0.001), significantly lower pain scores after the anesthesia by 2 and 3 hours (P < 0.001). Improved recovery after surgery resulted in increased same-day discharge rates and better perioperative outcomes without affecting 30-day morbidity in women undergoing laparoscopic minimally invasive nonhysterectomy gynecological procedures.16
Systematic reviews on enhanced recovery after gynecological procedures performed both as open surgery and as minimally invasive gynecological surgery (MIGS) presented an assessment of the advantages of this approach.6,17 The data were extracted from eligible studies, including change in quality of life and recovery over time, postoperative complications including nausea and vomiting, use of opioids or anesthesia, patient satisfaction, postoperative pain, and rate of readmission as outcomes. Many of the included studies reported significant reductions in readmission rates, hospital costs, postoperative nausea and vomiting, and clinically meaningful increases in patient satisfaction were noted.6,17,18
Hysterectomy itself is one of the most frequently performed surgeries in gynecological practice. At the same time, surgical stress initiates the development of a catabolic state, leading to loads on the cardiovascular system, causing relative tissue hypoxia, increased insulin resistance, disorders of blood coagulation profiles, and changes in the function of the lungs and gastrointestinal tract. According to current guidelines, enhanced recovery after surgery (ERAS) pathways have been developed to maintain normal physiology in the postoperative period, thus optimizing patient outcomes without increasing postoperative complications or rehospitalizations.19 The basic principles of ERAS are the following: preoperative counseling and nutritional strategies, including avoidance of prolonged postoperative fasting; postoperative care, including a focus on regional anesthesia and nonopioid analgesics, fluid balance, and maintenance of normothermia; and promotion of postoperative recovery strategies, including early mobilization and appropriate thromboprophylaxis. Benefits of ERAS pathways include shorter hospital stays, reduced postoperative pain and analgesia requirements, faster recovery of bowel function, lower rates of complications and readmissions, and increased patient satisfaction. These advantages have been replicated across the spectrum of gynecological surgeries, including open and minimally invasive approaches, benign and oncological surgeries.20,21
The research of Lashkul O. allowed to confirm the data that the usual methods of preoperative preparation (fasting, bowel lavage, long period of food restriction, significant decrease in motor activity, fluid loading), standard approaches to intraoperative management (predominance of general anesthesia, long-term catheterization of blood vessels and bladder, mandatory long-term drainage) and the postoperative period (use of opioids, infusion load, lack of prevention of nausea and vomiting, fasting) demonstrated insufficient efficiency, low quality of life of patients, development of stress and financial burden on society in general and the family in particular, in contrast to the method of the multimodal strategy of FTS, the advantages of which are a reduction in the level of pain, in the duration of bladder catheterization, early activation, objective and subjective improvement of the physical and psychological state of patients, and a decrease in the level of medication burden.1
A prospective longitudinal cohort study conducted by Nilsson L. et al. in five Swedish hospitals with a cohort evaluation of 162 women who underwent abdominal hysterectomy under a rapid treatment program, showed the development of postoperative complications in 25.3% of cases (mainly infection and impaired wound healing). Significant risk factors for postoperative complications were obesity (OR 8.83), previous laparotomy (OR 2.92) and relative weight gain on the first postoperative day (OR 1.52).22 According to Ferrari F. et al., the application of the enhanced recovery after surgery protocol in gynecological surgery leads to a reduction in patient length of stay regardless of the surgical access and the type of gynecological disorder.23
Carter-Brooks CM. et al. in the presented retrospective analysis of patients who underwent pelvic floor reconstructive surgery, compared same-day discharge, duration of hospitalization, and postoperative complications before and after the implementation of enhanced recovery after surgery at a tertiary hospital.24 The authors found no group differences in total 30-day postoperative complications overall and for the following categories: urinary tract infections, emergency department visits, unscheduled office visits, and returns to the operating room. Patients with enhanced recovery after surgery were more likely to be readmitted with weakness, chest pain, hyponatremia, wound complications, nausea/ileus, and ureteral obstruction. That is, improved recovery after surgery in urogynecological population resulted in a higher rate of same-day discharge and high patient satisfaction but with slightly higher 30-day readmissions.24
Thus, the analytically processed data of literary sources and the obtained results of this scientific search allow to make the following scientific propositions, which require further research and study.
Conclusions
Studies have demonstrated the feasibility of using laparoscopic technology in combination with the FTS technique, taking into account social and psycho-traumatic factors (concern about a long period of incapacity for work and loss of work, waiting for full or maximum recovery, including readiness for hard physical work). The specified optimized approach made it possible to evaluate the following positive aspects: minimal invasiveness, low risk of infectious complications, short courses of antibiotic therapy, mild postoperative pain, cosmetic effect, short hospitalization periods and quick recovery.
The obtained results demonstrate a decrease in the volume of intraoperative blood loss, which is positively reflected in a decrease in blood and fluid balance and creates prerequisites for reducing the volume of infusion and shortening the time of invasive intravascular intervention.
The analysis of the obtained results allows to single out transvaginal hysterectomy with laparoscopic assistance, using FTS-surgery protocols as the surgical technique of choice for the recovery of uterine leiomyoma patients of reproductive age and as the most effective way in terms of quality of life indicators.
The experience of using FTS-surgery protocols in gynecology during surgical recovery of women of reproductive age for uterine leiomyoma showed that the enhanced recovery technique allows to improve the course of the early postoperative period, reduce the postoperative pain syndrome, decrease the risk of intestinal paresis and shorten the rehabilitation period, and, as a result, improve indicators of quality of life.
References
- Lashkul OS., Havryliuk VP., Pavelko NO. Fast track surgery is a multimodal strategy for managing the postoperative period in gynecological patients. The role of an anesthesiologist. Clinical Anesthesiology and Intensive Care. 2017. 1(9):21–28.
- Cherniy VI., Yevseieva VV., Serbul MM. Perioperative management in bariatric surgery based on ERAS guidelines. Preventive and Clinical Medicine. 2019. 1(7):47-58. https://cp-medical.com/index.php/journal/article/view/54
- Yevsieieva V, Perehrestenko A, Kozubovich R. Does ultrasound-guided transversus abdominis plane blockade decrease perioperative opioids in morbid obese patients undergoing laparoscopic surgery? Wiadomosci Lekarskie (Warsaw, Poland : 1960). 2019 ;72(11 cz 1):2108-2112.
- Pylypenko, M., Bondar, M., & Khomenko, O. Perioperative management according to the principles of the program of rapid postoperative recovery (ERAS) in the prevention of acute bowel obstruction (a clinical lecture). EMERGENCY MEDICINE, 2022. 18(2), 34–38. https://doi.org/10.22141/2224-0586.18.2.2022.1471
- Chao L, Lin E, Kho K. Enhanced Recovery After Surgery in Minimally Invasive Gynecologic Surgery. Obstet Gynecol Clin North Am. 2022 Jun;49(2):381-395. doi: 10.1016/j.ogc.2022.02.014.
- Kalogera E, Glaser GE, Kumar A, Dowdy SC, Langstraat CL. Enhanced Recovery after Minimally Invasive Gynecologic Procedures with Bowel Surgery: A Systematic Review. J Minim Invasive Gynecol. 2019 Feb;26(2):288-298. doi: 10.1016/j.jmig.2018.10.016.
- Members of the Working Party; Nightingale CE, Margarson MP, Shearer E, Redman JW, Lucas DN, Cousins JM, Fox WT, Kennedy NJ, Venn PJ, Skues M, Gabbott D, Misra U, Pandit JJ, Popat MT, Griffiths R; Association of Anaesthetists of Great Britain; Ireland Society for Obesity and Bariatric Anaesthesia. Peri-operative management of the obese surgical patient 2015: Association of Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric Anaesthesia. Anaesthesia. 2015 Jul;70(7):859-76. doi: 10.1111/anae.13101
- Makarchuk OM., Havryliuk HM. Peculiarities of assessing the quality of life and finding ways of rehabilitation for women who had uterus surgery. Galician Medical Journal. 2016. 23(3)1:40-43.
- Tkachenko RO., Hrizhymalskyi YeV. Modern perioperative infusion therapy in obstetrics. Pain, anesthesia and intensive care: scientific and practical journal of the Association of Anesthesiologists of Ukraine, 2016. 1:11-18.
- Trowbridge ER, Dreisbach CN, Sarosiek BM, Dunbar CP, Evans SL, Hahn LA, Hullfish KL. Review of enhanced recovery programs in benign gynecologic surgery. Int Urogynecol J. 2018 Jan;29(1):3-11. doi: 10.1007/s00192-017-3442-0.
- Rodgers A, Walker N, Schug S et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ 2009; 321: 1–1
- Hrizhymalskyi YeV, Harha AI. Modern methods of pain relief in obstetrics and gynecology. Medical Aspects of Women’s Health, 2018. 4(117):30-35.
- Suresh V. Enhanced recovery after gynecologic surgery. Am J Obstet Gynecol. 2021 Mar;224(3):335-336. doi: 10.1016/j.ajog.2020.11.019.
- Chen Y, Fu M, Huang G, Chen J. Effect of the enhanced recovery after surgery protocol on recovery after laparoscopic myomectomy: a systematic review and meta-analysis. Gland Surg. 2022 May;11(5):837-846. doi: 10.21037/gs-22-168.
- Feng Q, Liao W, Feng X, Du J, Li J. Is enhanced recovery after surgery protocol has high value in after laparoscopic myomectomy? Gland Surg. 2022 Aug;11(8):1431-1432. doi: 10.21037/gs-22-334.
- Peters A, Siripong N, Wang L, Donnellan NM. Enhanced recovery after surgery outcomes in minimally invasive nonhysterectomy gynecologic procedures. Am J Obstet Gynecol. 2020 Aug;223(2):234.e1-234.e8. doi: 10.1016/j.ajog.2020.02.008.
- Marchand GJ, Coriell C, Taher A, King A, Ruther S, Brazil G, Cieminski K, Calteux N, Ulibarri H, Parise J, Arroyo A, Sainz K. Systematic review of the effect of implementing enhanced recovery after surgery on selected attributes of surgical recovery in gynecology. Turk J Obstet Gynecol. 2021 Sep 27;18(3):245-257. doi: 10.4274/tjod.galenos.2021.47717.
- Levy L, Tsaltas J. Recent advances in benign gynecological laparoscopic surgery. Fac Rev. 2021 Jul 26;10:60. doi: 10.12703/r/10-60. PMID: 34409423; PMCID: PMC8361750.
- ACOG Committee Opinion No. 750: Perioperative Pathways: Enhanced Recovery After Surgery. Obstet Gynecol. 2018 Sep;132(3):e120-e130. doi: 10.1097/AOG.0000000000002818.
- Nelson G, Dowdy SC. Level I evidence establishes enhanced recovery after surgery as standard of care in gynecologic surgery: now is the time to implement! Am J Obstet Gynecol. 2020 Oct;223(4):473-474. doi: 10.1016/j.ajog.2020.07.048.
- Trowbridge ER, Dreisbach CN, Sarosiek BM, Dunbar CP, Evans SL, Hahn LA, Hullfish KL. Review of enhanced recovery programs in benign gynecologic surgery. Int Urogynecol J. 2018 Jan;29(1):3-11. doi: 10.1007/s00192-017-3442-0.
- Nilsson L, Wodlin NB, Kjølhede P. Risk factors for postoperative complications after fast-track abdominal hysterectomy. Aust N Z J Obstet Gynaecol. 2012 Apr;52(2):113-20. doi: 10.1111/j.1479-828X.2011.01395.x.
- Ferrari F, Forte S, Sbalzer N, Zizioli V, Mauri M, Maggi C, Sartori E, Odicino F. Validation of an enhanced recovery after surgery protocol in gynecologic surgery: an Italian randomized study. Am J Obstet Gynecol. 2020 Oct;223(4):543.e1-543.e14. doi: 10.1016/j.ajog.2020.07.003.
- Carter-Brooks CM, Du AL, Ruppert KM, Romanova AL, Zyczynski HM. Implementation of a urogynecology-specific enhanced recovery after surgery (ERAS) pathway. Am J Obstet Gynecol. 2018 Nov;219(5):495.e1-495.e10. doi: 10.1016/j.ajog.2018.06.009.