Research Article
Chatzipapas I., Kathopoulis N., Protopapas A., Kyritsis N., Vlachos D. E., Loutradis D.
1st Department of Obstetrics and Gynecology, University of Athens, Alexandra Hospital, Athens, Greece
Correspondence: Chatzipapas Ioannis, Alexandra Hospital, 80 Vassilisis Sofias Avenue 115 28, Athens, Greece, E-mail: ixatzipapas@yahoo.gr
Abstract
Introduction: The purpose of this study was to evaluate the feasibility and clinical outcome of a new setup for cystoscopy using mobile technology. Materials and Methods: A total of 20 women with indications of cystoscopy were examined according to the new setup using smartphone and portable led light sources and the standard cystoscopic setup. The image quality as far as it concerns the ability to end up with a correct diagnosis was assessed. The total cost of the two setups was also compared. Results: The image reviews of the experts revealed no difference in the diagnostic adequacy of the two setups. All 40 reviews, regardless of device used for image capture were conclusive for the diagnosis. Moreover, the total price difference between the two devices was 46.401€ Conclusions: With the new system high quality images may be captured and it has the advantage of minimal equipment and easy set up. Moreover, the combination of portability and low cost could be a step towards universal cystoscopy after gynecological operations in order to induce the detection of urinary tract complications.
Keywords: Cystoscopy; portable cystoscope; smartphone; medical image; mobile
Introduction
Cystoscopy is the procedure utilized to visualize the lower urinary tract. The cystoscope is inserted into the urethra under direct vision and the walls of the urethra are visualized 1. The bladder neck, the trigone and the ureteral orifices are then observed and any pathology is revealed. Possible indications of cystoscopy are urgency-frequency syndrome, interstitial cystitis, intraoperative trauma, anatomical lesions, malignancy and catheter insertion. The majority of these pathologic entities is managed by Urologists, but all gynecologists should be capable of performing a cystoscopy 2.
During the past 2 decades gynecologists have become even more involved in evaluating urgency frequency syndrome and performing pelvic floor reconstruction procedures. Therefore ACOG in 2007 has recommended cystourethroscopy to be performed for diagnostic and a few operative indications by gynecologists• most importantly for ruling out cystotomy and intravesical or intraurethral suture or mesh placement, and for verifying ureteral patency 3. On the other hand cystoscopy is not always a part of the training in most gynecology residency programs, a fact that limits the expansion of this procedure in clinical practice 4. Moreover the cost of the equipment is highly elevated in a way that makes them inaccessible for many health care facilities.
Our department has developed a portable cystoscopy setup with the utilization of mobile smartphone, a specially designed adaptor and a portable light source. The mobile phone is transformed this way into a completely mobile cystoscopic viewing system and the whole setup portable.
Material and methods
Portable setup
In our study we used 2 different cystoscopy setups. A standard one using a rigid 30 degrees cystoscope coupled with an endoscopic camera (Karl Storz camera head), a video system/receiver monitor and a standard high powered xenon light source. The alternate was the same cystoscope coupled via a commercially available adaptor with an iPhone 6s (Apple Inc., Cupertino, CA) in camera mode. A portable light source has been used to make the system transportable. In addition to the smartphone display we used Apple TV and Airplay to wirelessly stream a mirrored display of the endoscopic image to a larger display. The smartphone contained no cellphone provider card and we only used its multimedia capabilities.
Cystoscopy technique
In our Department we perform diagnostic cystoscopy in selected vaginal and abdominal operation mostly TVT vaginal tapes for urine incontinence, vaginal hysterectomies and cancer staging (cervical). Moreover cystoscopy is also used for pigtail catheter placement to the ureters. Initially the patient is in the dorsal lithotomy position and the vaginal introitus is prepared with normal saline. Lidocaine hydrochloride 1% gel can be used as a local anaesthetic and lubricant. A rigid, 70° narrow caliber cystoscope is introduced into the urethra. We infuse normal saline at a pressure of 150 mmHg and we visualize the urethral wall and direct the cystoscope into the bladder. On entering the urinary bladder the cystoscope should be tilted downwards to enable the operator to visualise initially the neck and then the trigone of the urinary bladder. In case of intraoperative performance the patient is already under general or epidural anesthesia. In case of diagnostic cystoscopy there is no need for anesthesia, except the cases that a pigtail catheter must be introduced or replaced that the patient must be anesthetized (Figure 1, 2, 3).
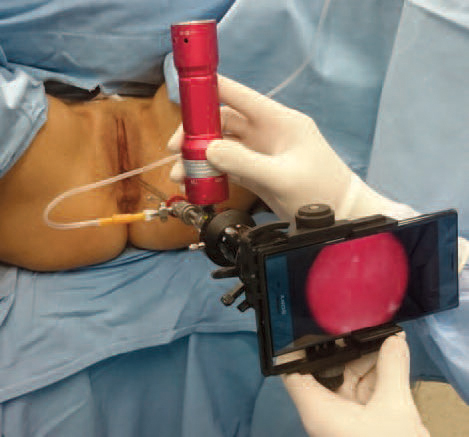
Figure 1. Portable cystoscopy set up. The rigid cystoscope coupled with smartphone and portable LED light source.
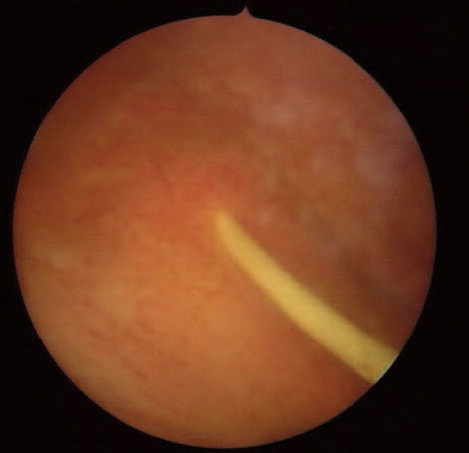
Figure 2. Pigtail catheter inside bladder (mobile image)

Figure 3. Pigtail catheter inside bladder (standard image)
Patient selection
Our study included 20 patients with benign or malignant gynecologic entities having the indication for diagnostic cystoscopy or pigtail catheter removal. Each one of the patients underwent cystoscopy with both setups and the images were collected and reviewed from 2 independent experts on the field. The patients have signed a written informed consent form and agreed to participate in this study. The study was approved by the local ethics committee. Each image has been rated from the evaluators based on Lickert analog scale (from 1 very poor quality to 5 very good quality) concerning the quality overall, the colors, the brightness and the resolution. The evaluators were blinded as to which set was from either device. Moreover the experts were questioned if any single’s image quality was adequate in order to make the diagnosis.
Results
When queried about the efficacy of the two setups concerning the performance of cystoscopy, the experts noted that both devices were convenient. The image reviews of the experts revealed no difference in the diagnostic adequacy of the two setups. The operators also stated that they faced no problems on pigtail catheter removal but as for catheter placement there were some difficulties that have to be overcome on how to keep the whole system sterilized. All 40 reviews, regardless of device used for image capture were conclusive for the diagnosis (Figure 4, 5, 6).

Figure 4. Atypical vascular lesions

Figure 5. Primary adenocarcinoma of the bladder

Figure 6. Atypical post-radiation vascular lesions
The cost of the standard medical camera system was 15.000€ and 18.000€ the monitor and video system. Moreover xenon light source’s cost is 15.000€; total cost of the standard setup is 48.000€. On the other hand iPhone 6s costs 699€ and 650€ the adaptor used. Another 250€ is the cost of the portable light source. Finally our new setup has a total cost of 1.599€. The total price difference between the two setups is 46.401€.
Discussion
Intraoperative cystoscopy for the detection of surgical trauma in bladder or ureters is a very useful procedure for the gynecologists. Rates of ureteral and bladder injury during abdominal and pelvic surgery depend on procedure type and gynecologic operations due to close proximity of the uterus to the bladder and ureters are responsible for the 75% of these injuries. Moreover almost 95% of urinary bladder injuries are recognized and fixed at the time of surgery 5. Cystoscopy can help surgeons to identify any bladder trauma by direct vision or by fluid leakage to the vagina during filling. In addition the proximity of the injury to the ureteral orifices and the urethra can be evaluated as well 6.
Rates of urinary tract injury during gynecologic procedures have varied by type of surgery and type of injury. For patients who underwent laparoscopic gynecologic operations urinary tract injury rate ranged from 0,02% to 1,7% 7. In laparoscopic pelvic surgery the incidence of ureteral injury varied between 1-2% with the majority of injuries occurring during Laparoscopic Assisted Vaginal Hysterectomy 8. Inappropriate use of electrocoagulation was the leading cause of the ureteral injuries. In laparoscopic hysterectomies the bladder injury rate is 0,05% to 0,66% 9. Abdominal hysterectomies also have a risk of ureteric injury from 1,7% for benign indication to 4% for malignancies 10. Finally bladder injury is very common in the form of perforation or trauma, when Tension free vaginal tapes are inserted (4,4-71%) 11. It is therefore well known that the urinary tract injury and the ureter specifically is what ‘the gynecologist fears most in the pelvis’.
Except form urinary tract injury primary prevention by means of formal preoperative evaluation and planning, it is very important if the accident happens to be able to detect the damage intraoperatively. When the injury is located during the operation, the surgeon can repair it immediately and reduce the risk of further complications, re-operation and litigation problems that may follow. Cystoscopy is one of the most valuable tools towards this direction.
A number of studies have shown that routine use of cystoscopy in gynecologic operations may induce the percentage of urinary trauma detection at the time of the operation. Vakilli et al have shown that universal cystoscopy after hysterectomy may detect up to 96% of urinary tract injuries intraoperatively12. Before cystoscopy only 12,5% of ureteral injuries and 35,3% of bladder injuries were detected. Moreover, in a systematic review Teeluckdharry et al. tried to determine the urinary tract injury rates with and without routine use of cystoscopy for patients who underwent any type of hysterectomy. They concluded that routine cystoscopy clearly increases the intraoperative detection rate of urinary tract injuries but it does not appear to have much effect on the postoperative injury detection rate 13. On the other hand Chi et al. examining the effects of universal cystoscopy policy after hysterectomy in their institution, concluded that this practice is associated with decreased delayed postoperative urologic complications (0,7% vs 0,1%) 14.
One of the major concerns in order to apply universal cystoscopy is the cost of the equipment that may reach up to 48.000€. The cystoscope, the camera the light source and monitor and video system are necessary for the operation. Moreover this setup is at least cumbersome as all these instruments weight a lot and need to be immobilized in a specific operating room. Our system provides not only portability but also low cost service and the hospital could have one of these in each operating room in order to perform easily cystoscopy each time a gynecological operation is in progress. The ability to carry on the system in a handbag, permits to the healthcare providers to transfer it from one theater to the other in a few minutes.
Delayed urologic injuries always have a negative impact on the total cost of the gynecologic operation. Hospital charges in case of a ureteral injury may are multiplied and is not welcomed from the insurance companies the patient and finally the surgeon. In an analysis from Visco et al, universal cystoscopy found to be cost-effective when the rate of ureteral injury exceeds 1,5% for hysterectomies 15. But this analysis only includes hospital charges and does no take account for collateral costs of patients pain, days lost from work, lawyers payments and patients possible inability.
Conclusions
Urinary tract injury is a major concern for all gynecologists performing pelvic operations. The associated socioeconomic and psychological costs could be reduced if universal cystoscopy could be applied and possible trauma could be identified intraoperatively. The cost of the set up is one of the reasons that cystoscopy is not available in every operating room. Our system with the low cost and the portability is another step towards the practice of universal cystoscopy with its positive effects.
References
1. Weinberger MW. Cystourethroscopy for the practicing gynaecologist. Clin Obstet Gynecol 1998;41:764–6.
2. Foon R, Elbiss H, Moran P. Cystoscopy for gynaeclogists. The Obstetrician and Gynecologist 2006;8:78-85.
3. ACOG Committee Opinion. Number 372. July 2007. The Role of cystourethroscopy in the generalist obstetrician-gynecologist practice. Obstet Gynecol. 2007;110(1):221-224.
4. Jacobs KM, Hernandez LH, Thomas TN, et al. Perceptions of posthysterectomy cystoscopy training in obstetrics and gynecology residency programs. Female Pelvic Med Reconstr Surg. 2015;21(2):66-9.
5. Mattingley RF, Thompson JD. Vesicovaginal fistulas. In: Rock JA, Thompson JD, editors. Te Linde’s Operative Gynecology. Philadelphia: Lippincott-Raven; 1992. p. 758
6. HurtW. Gynaecological injury to the ureters, bladder and urethra. In: Walters MD, Karram MM, editors. Urogynecology and Reconstructive Pelvic Surgery, 2nd edition. London: Mosby; 1999. p. 383–4.
7. Magrina JF. Complications of Laparoscopic Surgery. Clinical Obstetrics & Gynecology: 2015; 21(2):66-9.
8. Ostrzenski A, Radolinski B, Ostrzenska KM. A review of laparoscopic ureteral injury in pelvic surgery. Obstet Gynecol Surv. 2003 Dec;58 (12):794-9.
9. Adelman MR, Bardsley TR, Sharp HT. Urinary tract injuries in laparoscopic hysterectomy: a systematic review. J Minim Invasive Gynecol. 2014 Jul-Aug;21(4):558-66. doi: 10.1016/j.jmig.
2014.01.006.
10. Kiran A, Hilton P, Cromwell DA. The risk of ureteric injury associated with hysterectomy: a 10-year retrospective cohort study. BJOG. 2016 Jun;123(7):1184-91.
11. Atherton MJ, Stanton SL. The tension-free vaginal tape reviewed: an evidence-based review from inception to current status. BJOG 2005;112 :534–46.
12. Vakili B1, Chesson RR, Kyle BL, et al. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol. 2005 May;192 (5):1599-604.
13. Teeluckdharry B1, Gilmour D, Flowerdew G. Urinary Tract Injury at Benign Gynecologic Surgery and the Role of Cystoscopy: A Systematic Review and Meta-analysis. Obstet Gynecol. 2015 Dec;126(6):1161-9.
14. Chi AM, Curran DS, Morgan DM et al. Universal Cystoscopy After Benign Hysterectomy: Examining the Effects of an Institutional Policy. Obstet Gynecol. 2016 Feb;127(2):369-75.
15. Visco AG1, Taber KH, Weidner AC, et al. Cost-effectiveness of universal cystoscopy to identify ureteral injury at hysterectomy. Obstet Gynecol. 2001 May;97(5 Pt 1):685-92.
Received 28-4-2017
Revised 22-5-2017
Accepted 20-6-2017