Case Report
Ahmed Samy El-Agwany
Department of Obstetrics and Gynecology, Faculty of Medicine, Alexandria University, Egypt.
Correspondence: Ahmed S El-Agwany, El-shatby maternity university hospital, Faculty of Medicine, Alexandria University, Alexandria, Egypt, E-mail: Ahmedsamyagwany@gmail.com
Abstract
Background: Abnormal placental invasion has increased with persistent rise in Caesarean delivery. Management depends on accurate diagnosis and delivery should be planned at an institution with appropriate expertise and resources. Hemorrhage in pregnancy is the leading cause of maternal mortality in developing countries. Internal iliac artery ligation is one of the lifesaving procedures in intractable pelvic hemorrhage. The vascular malformations involving the abdominal aorta, common iliac artery and its branches are very rare. Case: We present a case of placenta accreta which is a major risk for peripartum deaths. In this case we try to explain our conservative surgical approach. Normally the abdominal aorta bifurcates into the right and left common iliac arteries anterolateral to the fourth lumbar vertebra. In the present case, there was bilateral absence of common iliac arteries which are the terminal branches of the abdominal aorta. Internal iliac artery was extremely long and equal size to external one. The reason for the absence of common iliac artery is attributed to the disappearance of the initial segment of the umbilical artery. Conclusion: Cesarean section and placenta previa are significant risk factors for placenta accreta whichis associated with high fetomaternal morbidity and mortality. In order to avoid postpartum hemorrhage and fertility loosing hysterectomy, our approach which consists of bilateral hypogastric arterial ligation and transverse compression sutures can be applied succesfully. Proper identification of anatomical variations in pelvic vasculature is essential for surgical and radiological interventions to prevent complications. This article aims at sharing author’s experience about usefulness of this surgical procedure in arrest of pelvic hemorrhage and to remove the inhibition among practicing gynecologists regarding this procedure.
Keywords: internal iliac artery; common iliac artery; compression suture; placenta accrete; ligation; cesarean section
Introduction
The incidence of placenta accreta is 1 per 2,500 deliveries worldwide and it occurs when there is a defect in decidua basalis, resulting in an invasive placentation1.Prior uterine surgery, myomectomy and curettage, in addition to caesarean section have are associated but placenta previa has been associated with a high rate1.
The maternal mortality about 7 % and the surgery related morbidities include massive transfusions, infections, urologic injuries and fistula formation2. Optimal management involves early recognition of high risk women and meticulous planning at the time of delivery.
One of the important methods of controlling pelvic hemorrhage is the ligation of internal iliac arteries. The procedure was performed for the first time by Kelly in 1893 during hysterectomy for uterine carcinoma3. In obstetrics, massive bleeding due to atonic or traumatic post-partum hemorrhage, adherent placenta and rupture uterus are the main indications4. Any obstetrician who attends and experiences a case of severe postpartum hemorrhage clearly understands the risk of losing a patient from hemorrhage. The memory will last forever.
Reported complications include inadvertent ligature of the common iliac artery, prolonged blood loss and prolonged operative time. It has also been reported that there is a high rate of complication and low rate of success for hemostasis if the procedure is not done correctly5. Therefore, this procedure should be reserved for hemodynamically stable patients of low parity in whom future child-bearing itself is of paramount concern. Unilateral or bilateral hypogastric artery ligation can be life-saving6. If the procedure is performed correctly, there is no morbidity, either short- or long-term with bilateral or unilateral ligation6.When it becomes obvious that conservative methods have failed, unilateral or bilateral internal iliac artery ligation should be considered urgently7.
The pelvic vasculature is arranged in such a manner that there is ample collateral circulation8. The common iliac artery bifurcates into two main branches – the external iliac artery (which becomes the femoral artery at the inguinal ligament) and the internal iliac (hypogastric) artery which descends into the true pelvis. The latter divides into anterior and posterior branches. It is essential to identify this division because the uterine artery branches off from the anterior division. Reich and co-workers in 19648 used dissection of fresh cadavers to show that numerous variations occur in the anatomy of these vessels. It is not always true, for example, that one or both of the internal iliac (hypogastric) branches are of similar diameter along the entire length. Therefore, visual observation alone can be misleading. Surgeons should therefore be aware of the fact that subdivision of the main internal iliac trunk may be into branches that are not significantly narrower than the main trunk.
Vascular malformations involving the iliac and femoral vessels are far more rare than thoracic and abdominal aorta9. The abdominal aorta bifurcates into the right and left common iliac arteries at the level of fourth lumbar vertebra10. Vascular malformations involving the iliac and femoral vessels are usually discovered incidentally. The exact prevalence of iliofemoral variations is unknown, but no more than 6 cases by angiography in a series of 8000 symptomatic patients9.
Complete absence of the common iliac artery specifically is an extremely rare anomaly. Mansfield and Howard showed the autopsy specimen of a patient with congenital bilateral absence of the common iliac arteries. In that case, the aorta divided directly into two internal iliac arteries and two external iliac arteries11. The present case showed bilateral absence of common iliac arteries.(Figure 1)
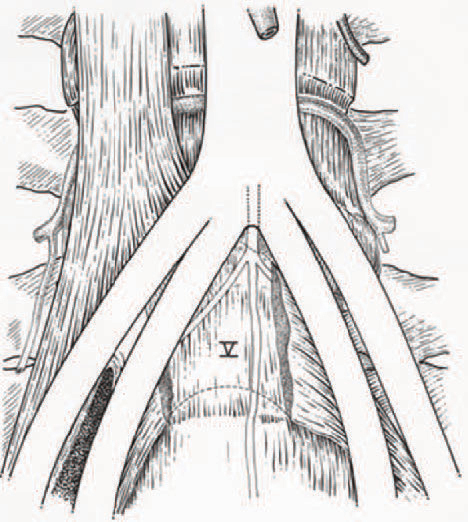
Figure 1. Adachi found a very short right common iliac artery the left common iliac artery was absent11
We present a case of extensive placenta accrete with placenta Previa in previous caesarean section in 22 y old female with fertility preserving surgery and bilateral internal iliac artery ligation that was abnormal. Common iliac arteries were absent bilaterally with internal iliac arteries so long. there is no data regarding this issue before so, this is the first case reported with this condition in pregnancy with ligation.
Case Report
A 22 years old woman who had pregnancy complicated by placenta previa and placenta accreta was referred to our university hospital. She had a history of twice caesarean section with one living child and the other was dead in utero with severe preeclampsia. Ultrasonographic examination at 27 weeks revealed the internal cervical os was covered completely by placenta with the placenta revealing multiple hypoechoic spaces (lacunae), turbulent internal flow and thinning of the myometrium with ill-defined uterovesical space and loss of retroplacental space. There was normal fetal growth with normal scan regarding gestational age the cervix was closed. These findings were interpreted as total placenta previa -accrete. the patient was followed closely till delivery. The patient was scheduled for an elective Caesarean section planning for conservative surgery for fertility sparing, at 38 weeks. The patient was informed about the risk of her condition and possible complications related to the procedure. Preoperatively hemoglobin was 12.5 g/dl. There was no bleeding attacks. All the coagulation profiles were found within normal range. Against the risk of bleeding and disseminated intravascular coagulation, four unit whole blood, 2 units platelet and 4 units of plasma were prepared according to our resources. the patient complained of labor pains and vaginal bleeding at 37 weeks and so, she was transferred to operating room for cesarean section. In the operating room, the abdomen was entered by large pfennesteil incision according to our hospital policy. High transverse uterine incision was done in order to avoid interruption of the placenta. Then, removal of fetus by breech extraction due to transverse lie was done. We waited for placental separation but could not be seen. Gentle traction was applied but failed. Placental invasion anomaly was confirmed surgically.
Manual removal of the placenta with piece meal extraction was done. Minimal placental tissues were cut. The myometrium was invaded by the placental tissue with extreme thinning difficult to differentiate from bladder wall. The uterine serosa was intact but adhesions with bladder were present. The main bulk of the placenta was mainly on the left side with deviation of the internal os to the right side that was identified before suturing. Bleeding in the cervical region was observed. sharp dissection of the bladder was done from a virgin area in the uterovesical space but iatrogenic injury about 1 cm occurred in the dome of the bladder. we continued dissection till exposing the whole lower segment. Transverse compression sutures were taken from down up till the incision line avoiding the internal os. The uterine incision was sutured .there was bleeding from the uterovescial pouch and the uterus so, we proceeded with internal iliac artery ligation.
Peritoneum on the lateral side of common iliac artery was vertically opened in such a way that the ureter remained attached to the medial fold. Internal iliac artery was traced downwards. The fascia over the artery was dissected away. Single thread of suture was passed beneath the artery with the help of right angle forceps .Once sufficient experience is gained, the time required for ligation is not more than 5 to 7 minutes after opening the abdomen. It’s a dictum that the artery is not ligated until the bifurcation of the common iliac artery is both palpated and visualized as there is no room for error. A variation was observed in the termination of the abdominal aorta. There was bilateral absence of the common iliac artery with both of its terminal branches (external and internal iliac arteries) arising directly from abdominal aorta at the level of L4. The internal was so long about 10 cm of near equal diameter caliber to the external iliac artery. It was ligated bilaterally 3 cm of the bifurcation after confirming pulsations in the femoral artery and visualizing the ureter clearly.
Bleeding arrested after wards .We repaired the bladder injury in 2 layers with 3/0 vicryl with insertion of 18 fr foley`s catheter in urethra for 10 days. We inserted 2 drains intraperitoneal and sub rectus sheath one she receive about one liter of blood with 2 units of plasma. Duration was about one and half hour. she received postoperative 2 units of blood. After 24 hours from the operation, 100cc of the tube was taken out. Antibiotics were administered at duration of Foley`s catheter insertion to reduce the risk of iatrogenic infection .Hemoglobin was about 9 gm%. She was discharged after 7 days with iron therapy for 6 month. The baby was male in good condition .
Transvaginally ultrasonography showed no placental residual mass in the uterus. Patient was followed in the puerperium period. Her beta human chorionic gonadotropin level was 5mUI/mL at the end of puerperium.
Discussion
Accreta vera is the most common form of placenta accrete accounting for 75–78 %, increta about 17 % while percreta about 5–7 % of all women12. Placenta previa and previous caesarean section are the two most significant risk factors associated as in our case. The earliest gestation at which placenta accreta was encountered is 8 weeks which was a caesarean scar pregnancy. There are reports of women when woman was taken up for dilatation and curettage, developed torrential hemorrhage necessitating hysterectomy and pathologic examination revealed accrete13. The woman continued pregnancy and underwent emergency cesarean hysterectomy at 37 weeks because of placenta increta14.
Currently the management options include conservative and extirpative approaches15. The conservative strategy entails leaving the placenta in situ which may be followed by medical management with methotrexate, uterine artery embolization, internal iliac artery ligation/embolization, dilatation and curettage or hysteroscopic loop resection16. However, risk of sepsis and delayed hemorrhage can occur. The radical approach consists of immediate cesarean hysterectomy, avoiding placental removal during operation.
Methotrexate recently, was argued that, after delivery of the fetus, the placenta is no longer dividing and therefore of no value17. Women had a high incidence of bleeding complications with an average blood loss of 2.7 l and as high as 19 U of blood and 21 U of FFPs were transfused18.
However some studies have shown conflicting results concerning the efficacy of prophylactic hypogastric artery ballooning, some have reported satisfactory outcomes19 and others have reported no benefit20 because of the rich collateral blood supply to the uterus.Bilateral hypogastric artery can be tied before separating the placenta in order to lower the bleeding after removing the placenta. Disseminated intravascular coagulation may also be avoided21.
Internal iliac artery ligation is an emergency life saving procedure that every pelvic surgeon must be able to perform. It is relatively simple operation, when performed by surgeon having adequate knowledge of pelvic anatomy. Internal iliac or hypogastric artery arises at the bifurcation of the common iliac arteries on either side at the level of the lumbosacral intervertebral disc and in front of sacroiliac joints, descends to the greater sciatic foramen for 3-4 cms where it divides into an anterior trunk which continues in line with the parent vessel towards the ischial spine and the posterior trunk which passes backwards towards the foramen.The main underlying principle in ligation of the internal iliac artery for control of pelvic hemorrhage is the conversion of an arterial pressure circulation into a venous pressure circulation. Unilateral ligation, decreases the pulse pressure distal to point of ligation by 77%,while bilateral ligation decreases the pulse pressure by 85%. As a result, blood clots begin to form. Blood supply to the pelvis continues via extensive collateral circulation with the aorta and the femoral artery .Collateral circulation becomes functional as early as 45-60 minutes after ligation. Little difficulty is encountered in palpating the pulsations of iliac vessels through the peritoneum in cases of hypovolemic shock. The vessel can be traced downwards from its origin. Unfortunately, the procedure is not popularly performed by many qualified surgeons doing pelvic surgery. The probable reasons are, lack of confidence in doing the procedure and fear of complications. Postgraduate training programme must include orientation of trainees to this life saving procedure22,23.
The reported success rate of IIAL varies from 40 to 100%, 24.Failures were more evident in atonic PPH than in other causes of PPH20. The failure is attributed to the technical difficulties and time required to block blood flow. Furthermore, because blood flow in the branches of the external iliac artery ascending from the perivesical area and in the vagina are so plentiful in cases of placenta increta or percreta, ligation of the internal iliac artery might be ineffective25. Furthermore, even if the internal iliac artery is ligated, peripheral arteries anastomose with the external iliac, inferior epigastric, and inferior mesenteric arteries that may supply blood to the uterus via uterine arteries.
In two-thirds of a large number of cases, the length of the internal iliac varied between 2.25 and 3.4 cm; in the remaining third it was more frequently longer than shorter, the maximum length being about 7 cm. the minimum about 1 cm. The lengths of the common iliac and internal iliac arteries bear an inverse proportion to each other, the internal iliac artery being long when the common iliac is short, and vice versa. The place of division of the internal iliac artery varies between the upper margin of the sacrum and the upper border of the greater sciatic foramen. The right and left hypogastric arteries in a series of cases often differed in length, but neither seemed constantly to exceed the other26.
Internal iliac artery is approximately 4 cm long. Bergman (1988) has reported that, internal iliac artery may be longer or shorter than usual. The branches may arise without the artery dividing into anterior and posterior division. Branches of the anterior and posterior divisions may exchange origins27,28.
The IIA is known to show some variations in its branching pattern and the knowledge of these variations is of utmost importance for the surgeons performing obstetric and gynecological surgeries29. According to Williams et al. and Naveen et al., the IIA arises at the level of the L5-S1 and divides into anterior and posterior divisions at the level of superior edge of greater sciatic notch30.According to the study of Mamatha et al which was done on 50 human cadaveric, the origin of the IIA at the level of L5-S1 was seen in72 %, at the level of S1 in 24 %, and at the level of L5 in 4 %31.
Complete absence of the common iliac artery specifically is an extremely rare variation. Mansfield and Howard showed the autopsy specimen of a patient with congenital bilateral absence of the common iliac arteries. In their case study, the aorta divided directly into two internal iliac arteries and two external iliac arteries32. Dumanian et al. presented a case report of a 44-year-old man with long standing bilateral intermittent claudication secondary to congenital absence of the left common iliac, both external iliac and femoral arteries33. More recently, Llauger et al. described congenital absence of right common iliac artery in an asymptomatic patient in whom the blood supply to the right pelvis and the right lower extremity derived from a variant artery originating from the left hypogastric artery34. Dabydeen et al. reported a case of complete absence of the right common iliac artery in a 21-year-old woman, incidentally discovered by CT during the investigative procedure for acute abdominal pain. A network of prominent collateral arteries reconstituted the distal portion of the right external iliac artery and the common femoral artery, forming the arterial supply of the right lower limb. The initial segment of the umbilical artery becomes the common iliac artery. It is likely that the absence of common iliac artery is due to the disappearance of the initial segment of the umbilical artery35,36.
This case highlighted the importance of absent or short common iliac arteries in obstetrics especially in ligation of internal iliac artery in emergencies. There is no other cases reported in the literature regarding this anomaly. We encourage others to report their experience. There is no data confirming any abnormalities in the internal iliac artery ligation in any variation, and for that reason we proceeded with ligation after confirming its origin. We could not correlate if there is an association of this anomaly with poor placentation regarding bad obstetrics history of preeclampsia with loss of baby or even the poor blood supply to the uterus with placenta previa and acrreta in the present We wish others to examine these items furtherly to detect if any possible association especially that reported cases were with atherosclerosis.
Conclusion
Placenta accreta is increasing and previous caesarean section and placenta previa are important risk factors. Early preoperative diagnosis in the suspected women is the key to save the woman’s life. Adherent placenta should be suspected even in first trimester in women with known high risk factors who are undergoing evacuation. Manual placental removal may be needed for correct diagnosis. On the other hand, an accurate preoperative diagnosis could avoid manual placental removal. In order to avoid postpartum hemorrhage and hysterectomy, our approach which consists of bilateral hypogastric arterial ligation and transverse compression suture can be applied successfully. Pelvic surgeons must get out of fear for the technical considerations. Although, it may not always be effective in control of pelvic hemorrhage, it is more conservative procedure than obstetric hysterectomy in young women with intractable pelvic hemorrhage. The present case is an observation where there was bilateral absence of common iliac artery. Congenital absence of the iliac arteries is rare; it should be suspected in failure to detect the internal iliac in its lower position and when there is 4 major branches from the aorta. We should scan the aorta down to exclude this anomaly.
Funding
This study was not funded.
Conflict of Interest
All authors has nothing to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patient included in the study.
References
1. ACOG Committee on Obstetric Practice. Committee opinion no. 266: placenta accreta. Obstet Gynecol. 2002;99:169–70.
2. O’Brien JM, Barton JR, Donaldson ES. The management of placenta percreta: conservative and operative strategies. Am J Obstet Gynecol. 1996;175:1632–8.
3. Kelly H. A. Ligation of both internal iliac arteries for hemorrhage in hysterectomy for carcinoma uterus. Bull. Johns Hopkins Hospital 1893; 5:53.
4. Bangal V, Kwatra A, Raghav S. Role of internal iliac artery ligation in control of pelvic hemorrhage. Pravara Med Rev 2009; 1(2)
5. Evans S, McShane P. The efficacy of internal iliac artery ligation in obstetric hemorrhage. Surg Gynecol Obstet 1985;160:250–3
6. Clark SL, Phelan JP, Yeh S-Y, et al. Hypogastric artery ligation for obstetric hemorrhage. Obstet Gynecol 1985;66:353–6
7. Shafiroff BGP, Grillo EB, Baron H. Bilateral ligation of hypogastric arteries. Am J Surg 1959;98:34
8. Reich WJ, Nechtow MJ, Keith L. Supplementary report on hypogastric artery ligation in the prophylactic and active treatment of hemorrhage in pelvic surgery. Int Surg 1965;44:1
9. Dabydeen D, Shabashov A, Shaffer K. Congenital absence of the right common iliac artery. Radiology Case Reports. 2008; 3.
10. Standring S, ed. Gray’s Anatomy. 39th Ed., Edinburgh, Elsevier Churchill Livingstone. 2005; 1360.
11. Mansfield AO, Howard JM. Absence of both common iliac arteries. A Case report. Anat Rec. 1964 Dec;150:363-4.
12. Jwarah E, Wilkin DJ. Conservative management of placenta accreta. J Obstet Gynaecol. 2006;26:378–9.
13. Comstock CH, Lee W, Vettraino IM, et al. The early sonographic appearance of placenta accreta. J Ultrasound Med. 2003;22: 19–23.
14. Chen YJ, Wang PH, Liu WM, et al. Placenta accreta diagnosed at 9 weeks’ gestation. Ultrasound Obstet Gynecol. 2002;19:620–2.
15. Kayem G, Davy C, Goffinet F, et al. Conservative versus extirpative management in cases of placenta accreta. Obstet Gynecol. 2004;104:531–6.
16. Mussalli GM, Shah J, Berck DJ, et al. Placenta accreta and methotrexate therapy: three case reports. J Perinatol. 2000;20: 331–4.
17. Morken NH, Kahn JA. Placenta accreta and methotrexate treatment. Acta Obstet Gynecol Scand. 2006;85:248–50.
18. Aggarwal et al. Morbidly Adherent Placenta: A Critical Review. The Journal of Obstetrics and Gynecology of India 2012; 62(1):57–61
19. Kidney DD, Nguyen AM, Ahdoot D, Bickmore D, Deutsch LS, MajorsC. Prophylactic perioperative hypogastric artery balloon occlusion abnormal placentation. AJR Am J Roentgenol 2001; 176: 1521-1524.
20. Greenberg JI, Suliman A, Iranpour P, Angle N. Prophylactic balloon occlusion of the internal iliac arteries to treat abnormal placentation: a cautionary case. Am J Obstet Gynecol 2007; 197: 471-744.
21. Karatke et al. Fertility sparing surgery on placenta invasion anomalies and placenta previa. Iranian Journal of Reproductive Medicine 2012; 10(3):271-274
22. Purandhare C. N. Internal iliac artery. Journal Obstet.Gynae. India 2002;52(4):21-22.
23. Parulekar S, Operative Gynaecology and Obstetrics, 3rd ed .Mumbai: Vora Medical publications,2003:377.
24. Murayama Y, Iwata A, Itakura A, Baba K, Seki H, Takeda S. A study on surgical management to control massive hemorrhage at caesarean hysterectomy for placenta previa accreta; balloon occlusion of common iliac arteries vs. conventional methods. Gynecologic Obstetric Surg 2008; 19: 111–116.
25. Vedantham S, Godwin SC, McLucas B, Mohr G. Uterine artery embolization: An underused method of controlling haemorrhage. Am J Obstet Gynecol 1997; 176: 938–948.
26. Atsushi Iwata et al. Limitations of internal iliac artery ligation for the reduction of intraoperative hemorrhage during cesarean hysterectomy in cases of placenta previa accrete. J. Obstet. Gynaecol 2010; 36(2): 254–259
27. Moore KL & Agur AM. Essential Clinical Anatomy Lippincott, 2 ed. 2002:224
28. Bergman RA, Thompson SA, Afifi AK and Saadeh FA. Compendium of human anatomic variation. Baltimore and Munich : Urban and Schwazenberg; 1988:84-85
29. Pavan P Havaldar, Sameen Taz, Angadi A.V, Shaik Hussain Saheb. Study of posterior division of internal iliac artery. Int J Anat Res 2014, 2(2):375-79. ISSN 2321-4287
30. Morita S, Saito N, Mitsuhashi N. Variations in internal iliac veins detected using multidetector computed tomography. Acta Radiologica. 2007; 48(10): 1082-5.
31. Naveen NS, Murlimunjo BV, Kumar V, Jayanthi KS, Rao K, Pulakunta T. Morphological analysis of the human internal iliac artery in South Indian population. Online Journal of Health and Allied Sciences. 2011; 10(1): 1-4.
32. Mansfield AO, Howard JM. Absence of both common iliac arteries. A Case report. Anat Rec. 1964; 150: 363–364.
33. Dumanian AV, Frahm CJ, Benchik FA, Wooden TF. Intermittent claudication secondary to congenital absence of iliac arteries. Arch Surg. 1965; 91: 604–606.
34. Llauger J, Sabate JM, Guardia E, Escudero J. Congenital absence of the right common iliac artery: CT and angiographic demonstration. Eur J Radiol. 1995; 21: 128–130.
35. Senior HD. The development of the arteries of the human lower extremities. Am J Anat 1919; 25: 54–95. Leriche R, Morel A. Syndrome of thrombotic obliteration of aortic bifurcation. Ann Surg. 1948; 127: 193–206.
36. Shailaja SHETTY et al. Bilateral absence of common iliac artery – a cadaveric observation. International Journal of Anatomical Variations 2013;6: 7–8
Received 12-5-2017
Revised 30-5-2017
Accepted 18-6-2017