Case Report
Thanasas K. Ioannis, Papavasileiou Sofia
Department of Obstetrics – Gynecology of General Hospital in Trikala, Trikala, Greece
Correspondence: Ioannis K. Thanasas, MD, MSc Efkli 33, 42100 Trikala, Greece, Tel: 2431029103 / 6944766469 E – Mail: hanasasg@hotmail.com
Abstract
The abdominal wall is the most common position locating endometriosis. The presentation of the event concerning the occurrence of endometriosis in scar of laparotomy after cesarean section. A patient, four years after cesarean section performed with Pfannestiel, came to our outpatient clinic with abdominal pain primary located in the left end of the surgical scar. Based on history and clinical findings was the suspected endometriosis of the abdominal wall and decided that surgical exploration of the disease. Intraoperatively was found hard clumps, a surface of which was solid adherent to the fascia of the abdominal muscles without good infiltration of the muscular wall. Histological examination of surgical preparation confirmed diagnosis of endometriosis in the abdominal wall with fresh bleeding and old data. In this work, after the description of the incident by the systematic arrangement and processing of modern references attempted a brief review of this rare localization of the disease, regarding the pathogenesis, diagnosis, treatment and prognosis.
Keywords: endometriosis, laparotomy scar, pathogenesis, diagnosis, treatment, prognosis
Introduction
Endometriosis first described by Rokitansky in 1860. It is a non – invasive neoplastic disease of the reproductive age of women, characterized by the presence and development of functional endometrial tissue outside of the normal anatomical limits of the uterus. The incidence of the disease is not easy to determine with precision. Overall, it is estimated that affects about 1% – 2% of women of reproductive age, approximately 40% – 60% of women with dysmenorrhea and 15% – 25% of infertile women1. Endometriosis is usually located in the bowels of pelvic and peritoneum. More rarely, it is possible to find and except pelvis spot disease in every tissue and organ in the female body, including laparotomy scar, episiotomy scar, navel, vagina, urinary, gastrointestinal, respiratory, central nervous system, and other2.
Case report
Patient 28 years old came to our clinic outpatient clinic with abdominal pain primary located in the left iliac fossa. The patient described the symptom from four years, about four months after performing caesarean section. Over time reported deterioration of its situation especially during the days of menstruation, when describing pain intensity greater while felt painful swelling of the skin in the area of the fault. The information received from the obstetrical history attesting to perform caesarean section Pfannestiel without postoperative complications. The medical history was free. By the clinical examination was found palpable painful induration at the left end of the surgical scar. After ultrasound of upper and lower abdomen there were no findings suggestive of intra-abdominal disease. The CT scan was without pathological findings. The levels of cancer antigen Ca125 were within normal limits.
Based on history and clinical findings was suspected endometriosis of the abdominal wall and decided that surgical exploration of the disease. Intraoperatively was found solid round mass, diameter about 4 cm, hard, small area which was solid adherent to the fascia of good abdominal muscles (Figure 1). There wasn’t found infiltration of the abdominal muscle wall. Histological examination of the preparation confirmed diagnosis of endometriosis in the abdominal wall with fresh and old bleeding elements (Figure 2). Postoperatively the patient reported relief of symptoms. No further therapeutic intervention established since it was considered that there was complete resection of endometriosis outbreak of the abdominal wall.
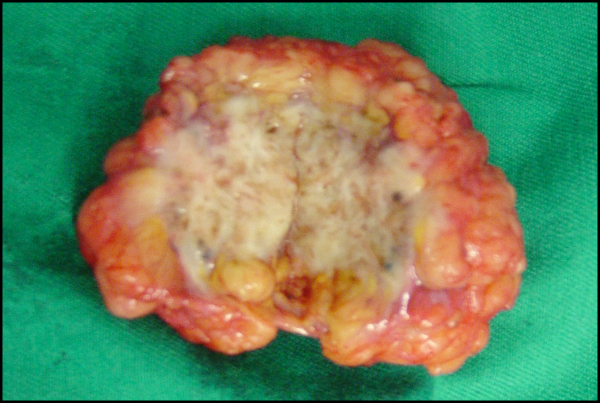
Figure 1. Macroscopic appearance ectopic endometriosis tissue in laparotomy scar after cesarean section (our case).
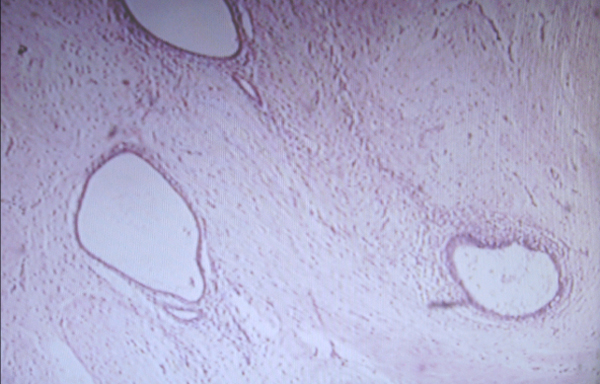
Figure 2. Microscopic view ectopic endometriosis tissue in laparotomy scar after cesarean section (our case).
Discussion
The abdominal wall is the most common place of development of ectopic endometriosis tissue. The lesion usually relates to the subcutaneous tissue, while rarely possible to expand the fascia abdominal muscles and muscle wall3. Although the literature cases automatic event reported the disease without prior open or laparoscopic surgery4, in most cases endometriosis of the abdominal wall is iatrogenic and related to previous surgery scar that requires the opening of the uterine cavity. The most important predisposing factor for the development of ectopic endometriosis tissue in the abdominal wall by the foregoing hysterectomy in pregnant women. Especially the destructible early pregnancy seems predisposed to implant the surgical scar. Generally, the frequency of development of the disease is estimated to be higher after uterine incision for terminating a pregnancy than after cesarean section. More specifically, after uterine incision to address second trimester abortion calculated terms in 1.08% of cases, and after cesarean 0.03% – 0.04%5. Recently, Chang and his colleagues showed that after cesarean section scar endometriosis in the laparotomy scar is related to 0.03% – 0.47% of cases, while the average period until onset of symptoms is estimated to be 39.3 months.6 Moreover, various gynecological surgeries open or laparoscopic access, and rarely amniocentesis (Table 1) included in predisposing factors have been implicated in endometriosis of abdominal wall7,8.
The diagnosis of endometriosis in surgical scars is not easy and often arises late. The symptoms are not specific and frequently appear after months or years after surgery. Usually displayed a slowly growing painful palpable mass in the scar area which may increase in size and become more painful during menstruation. The pain is the predominant symptom and occurs in almost all cases. The pain, though classically described as a periodic but by recent bibliographical almost half patients do not exhibit periodicity in pain9. Pain during menstruation may even get the form acute abdomen10. Severe pain may be the result of autonomous functional ectopic endometrial tissue with sensory nerves that contributes not only to a worsening of symptoms, but also in maintaining ectopic development11. The difficulty and delay diagnosis mainly due to scarcity of the disease, but also to a wide range of pathological conditions (Table 2) to be included in the differential diagnosis of endometriosis of the abdominal wall12.
Although the diagnosis preoperatively based strictly on history and clinical examination should not be denied the utility of laboratory tests and of modern imaging and interventional diagnostics (Table 3). The use today of serological markers, in addition to the early detection enables the proper postoperative monitoring, monitoring of disease response to the medication and to prevent possible recurrence or malignancy of the lesion. The more meaningful indicator is the cancer antigen 125 (Ca125), increase of which more than 1000 UI / ml may indicate the existence of invasive disease13. The diagnostic value of the Ca125 the early stages of endometriosis is very low, with specificity of between 83% – 93% and sensitivity starts at only 24% (24% – 94%)14. Recently, in the attempt to increase the diagnostic value of the Ca125 appear to contribute significantly and the concomitant use of other serological markers, such as cancer antigen 19 – 9 (Ca19 – 9)15, cancer antigen 15 – 3 (Ca15 – 3)16, various cytokines (IL – 6, TNF – a)17, P45014 aromatase14 and vascular endothelial growth factor (Vascular Endothelial Growth Factor – VEGF)18,19.
Ultrasound examination seems to be a useful but non-specific diagnostic method. With transabdominal ultrasound can been detected in the abdominal wall, the ultrasonographic characteristics which include a infrasound heterogeneous structure with internal echogenic echoes with irregular margins, often infiltrating the adjacent tissues20. Although ultrasound check cannot detect the peritoneal endomitriosical implants, the use of transvaginal sonography today is useful in investigation of pelvic structures, to determine the coexistence of pelvic desease21. With earlier study by Wolff and colleagues showed that 25% of women with endometriosis in laparotomy scar after cesarean section coexisted a pelvic desease22. Computed tomography and particularly magnetic resonance imaging outweigh ultrasound as it is able to provide valuable information on the location, depth, extent of damage and the possible infiltration of adjacent tissues from ectopic endomitriosic area23,24.
Unlike imaging, the aspiration biopsy with thin needle (Fine Needle Aspiration – FNA) can be a valuable and reliable diagnostic tool in the investigation of palpable masses in the abdominal wall. The method can distinguish ectopic endometrium from other pathologies included in the differential diagnosis of endometriosis of the abdominal wall and contribute to timely and accurate preoperative diagnosis, in order to achieve the most appropriate therapeutic approach design desease25 .
The treatment of endometriosis of the abdominal wall depends on the severity of symptoms and the age of the patient. Wide surgical resection of ectopic endomitriosic outbreak remains the treatment of choice, even for repeated recurrent lesions. It is usually curative, and also ensuring the confirmation of diagnosis. Intraoperatively, it is necessary to thorough cleaning of adjacent tissue damage in order to minimize the chances of relapse of the disease. If the symptoms are mild and the patient is to gestate in the near future, the surgical removal of the lesion should be carried out during cesarean26. Contrary to the surgical treatment, administration of hormonal preparations as first treatment appears to offer only temporary relief of symptoms. The role of conservative treatment in endometriosis of the abdominal wall is combined with surgical resection of the area of those cases of suspected excision of the lesion on unhealthy limits in order to avoid the increased risk of relapse The role of conservative treatment in endometriosis of the abdominal wall is combined with surgical resection of the area in those cases of suspected excision of the lesion on unhealthy limits in order to avoid the increased risk of relapse27. Finally, new therapeutic techniques that intend to reduce vascularization of ectopic endometrial tissue have been proposed and expected future to expand the available therapeutic options for the effective treatment of endometriosis, especially pelvic form of the desease28.
The prognosis of endometriosis of the abdominal wall is usually good. Immediately after surgery most patients report relief of their symptoms. Postoperative monitoring to determine Ca125 is necessary. The Ca125 a recurrence rate of the disease, and malignancy, as reported in the international literature incipient tumor masses endomitriosic origin in surgical scars after gynecological surgeries or caesarean29,30.
Conclusion
Endometriosis of the abdominal wall is generally iatrogenic. It is a rare form extra pelvic endometriosis in the differential diagnosis which should include all the painful masses in the abdominal wall. The cyclical changes, the progressive increase in the size of the lesion and a range of modern serological and imaging now permit early detection and the proper selection of the most appropriate therapeutic manipulations in order to minimize the risk of recurrence and to prevent malignant transformation of the disease.
References
1. Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J Assist Reprod Genet. 2010; 27: 441 – 447.
2. Machairiotis N, Stylianaki A, Dryllis G, Zarogoulidis P, Kouroutou P et al. Extrapelvic endometriosis: a rare entity or an under diagnosed condition? Diagn Pathol. 2013; 8: 194.
3. Bektaş H, Bilsel Y, Sari YS, Ersöz F, Koç O, et al. Abdominal wall endometrioma; a 10 –year experience and brief review of the literature. J Surg Res. 2010; 164: e77 – 81.
4. Chatzikokkinou P, Thorfinn J, Angelidis IK, Papa G, Trevisan G. Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatovenerol Alp Panonica Adriat 2009; 18: 126 – 130.
5. Patterson GK, Winburn GB. Abdominal wall endometriosis: report of 8 cases. Am Surg 1999; 65: 36 – 39.
6. Chang Y, Tsai EM, Long CY, Chen YH, Kay N. Abdominal wall endometriosis. J Reprod Med 2009; 54: 155 – 159.
7. Emre A, Akbulut S, Yilmaz M, Bozdag Z. Laparoscopic trocar port site endometriosis: a case report and brief literature review. Int Surg. 2012; 97: 135 – 139.
8. Hughes ML, Bartholomew D, Paluzzi M. Abdominal wall endometriosis after amniocentesis. A case report. J Reprod Med 1997; 42: 597 – 599.
9. Ozel L, Sagiroglu J, Unal A, Unal E, Gunes P, et al. Abdominal wall endometriosis in the cesarean section surgical scar: a potential diagnostic pitfall. J Obstet Gynaecol Res. 2012; 38: 526 – 530.
10. Gajjar KB, Mahendru AA, Khaled MA. Caesarean scar endometriosis presenting as an acute abdomen: a case report and review of literature. Arch Gynecol Obstet. 2008; 277: 167 – 169.
11. Kocakusak A, Aspinar E, Arikan S, Demirbag N, Tarlaci A, et al. Abdominal wall endometriosis: a diagnostic dilemma for surgeons. Med Princ Pract 2005; 14: 434 – 437.
12. Pachori G, Sharma R, Sunaria RK, Bayla T. Scar endometriosis: Diagnosis by fine needle aspiration. J Cytol. 2015; 32: 65 – 67.
13. Ghaemmaghami F, Karimi Zarchi M, Hamedi B. High levels of CA125 (over 1000 IU/ml) in patients with gynecologic disease and no malignant conditions: three cases and literature review. Arch Gynecol Obstet 2007; 276: 559 – 561.
14. Bedaiwy MA, Falcone T. Laboratory testing for endometriosis. Clin Chim Acta 2004; 340: 41 – 56.
15. Kurdoglu Z, Gursoy R, Kurdoglu M, Erdem M, Erdem O, et al. Comparison of the clinical value of CA 19 – 9 versus CA 125 of the diagnosis of endometriosis. Fertil Steril 2009; 95: 1761 – 1763.
16. Canda MT, Demir N, Sezer O, Doganay L. Successful treatment of advanced endometriosis with extremely high CA 125 and moderately elevated CA 15 – 3 levels. Clin Exp Obstet Gynecol 2008; 35: 231 – 232.
17. Othman Eel – D, Hornung D, Salem HT, Khalifa EA, El – Metwally TH, et al. Serum cytokines as biomarkers for nonsurgical prediction of endometriosis. Eur J Obstet Gynecol Reprod Biol 2008; 137: 240 – 246.
18. Altinkaya SO, Ugur M, Ceylaner G, Ozat M, Gungor T, et al. Vascular endothelial growth factor + 405 C/G polymorphism is highly associated with an increased risk of endometriosis in Turkish women. Arch Gynecol Obstet. 2011; 283: 267 – 272.
19. Liu F, Wang L, Zhang XX, Min SY, et al. Vascular endothelial growth factor receptor-2 inhibitor cediranib causes regression of endometriotic lesions in a rat model. Int J Clin Exp Pathol. 2015; 8: 1165 – 1174.
20. Hensen JH, Van Breta Vriesman AC, Puylaert JB. Abdominal wall endometriosis: clinical presentation and imaging features with emphasis on sonography. Am J Roentgenol 2006; 186: 616 – 620.
21. Brosens J, Timmerman D, Starzinski – Powitz A, Brosens I. Noninvasive diagnosis of endometriosis: the role of imaging and markers. Obstet Gynecol Clin North Am 2003; 30: 95 – 114.
22. Wolf YI, Haddad R, Werbin N, Skornick Y, Kaplan O. Endometriosis in abdominal scars: a diagnostic pitfall. Am Surg 1996; 62: 1042 – 1044.
23. Hassanin – Negila A, Cardini S, Ladam – Marcus V, Palot JP, Diebold MD, et al. Endometriomas of the abdominal wall: Imaging findings. J Radiol. 2006; 87: 1691 – 1695.
24. Busard MP, Mijatovic V, van Kuijk C, Hompes PG, van Waesberghe JH. Appearance of abdominal wall endometriosis on MR imaging. Eur Radiol. 2010; 20: 1267 – 1276.
25. Dash S, Panda S, Rout N, Samantaray S. Role of fine needle aspiration cytology and cell block in diagnosis of scar endometriosis: A case report. J Cytol. 2015; 32:71 – 73.
26. Teng CC, Yang HM, Chen KF, Yang CJ, Chen LS, et al. Abdominal wall endometriosis: an overlooked but possibly preventable complication. Taiwan J Obstet Gynecol 2008; 47: 42 – 48.
27. Momoeda M, Harada T, Terakawa N, Aso T, Fukunaga M, et al. Long – term use of dienogest for the treatment of endometriosis. J Obstet Gynaecol Res 2009; 35: 1069 – 1076.
28. Nisolle M, Alvarez ML, Clombo M, Foidart JM. Pathogenesis of endometriosis. Gynecol Obstet Fertil 2007; 35: 898 – 903.
29. Stevens EE, Pradhan TS, Chak Y, Lee YC. Malignant transformation of endometriosis in a cesarean section abdominal wall scar: a case report. J Reprod Med. 2013; 58: 264 – 266.
30. Dobrosz Z, Paleń P, Stojko R, Właszczuk P, Niesłuchowska – Hoxha A, et al. Clear cell carcinoma derived from an endometriosis focus in a scar after a caesarean section–a case report and literature review. Ginekol Pol. 2014; 85: 792 – 795.
Received 28-9-2017
Revised 15-10-2017
Accepted 28-10-2017