Research Article
Daniilidis A1, Balaouras D1, Chitzios D1, Sardeli C2, Mamopoulos A3, Assimakopoulos E1
12nd University department of Obstetrics and Gynecology, Hippokratio General Hospital, Aristotle University of Thessaloniki, Greece
2School of Medicine, Department of Pharmacology, Aristotle University of Thessaloniki, Greece
33rd University department of Obstetrics and Gynecology, Hippokratio General Hospital, Aristotle University of Thessaloniki, Greece
Correspondence: Angelos Daniilidis, 9 Smirnis , 56224, Evosmos, Thessaloniki, Greece, E-mail: info@gynekologia.gr
Abstract
Aim: To assess the diagnostic efficiency of TVS (transvaginal ultrasound measurement) for discrimination between benign and malignant endometrial conditions in asymptomatic postmenopausal women. Moreover, to evaluate the cut off risk for endometrial cancer in postmenopausal women, as a screening tool. Materials and Methods: In order to identify all studies related to the systematic review question, a detailed search strategy that took into account all important aspects of the clinical question and an appropriate study design, was developed. Two reviewers independently assessed study characteristics, methodological details and eligibility. Search strategy for evidence included 2 major medical databases PubMed and Cochrane Database of Systematic Reviews. Key words used were: asymptomatic postmenopausal women, atypical hyperplasia, endometrial cancer, transvaginal ultrasound, screening, endometrial thickening. Results: The significance of the thickness of the endometrium beyond 4 mm is not the same as for symptomatic postmenopausal women, and extrapolating guidelines from postmenopausal bleeding to asymptomatic population is not valid. In asymptomatic postmenopausal women, the risk of cancer is approximately 6.7% when endometrium is >11mm, which is comparable to the 5% risk in symptomatic postmenopausal women for a 5mm cut-off. If endometrium measures ≤11mm endometrial biopsy is not necessary. A postmenopausal asymptomatic woman with known risk factors for endometrial cancer like diabetes, obesity, use of unopposed estrogen or tamoxifen, will have a higher risk of cancer even with the same TVS measurement. The diagnostic accuracy of hysteroscopy was optimal for all intra-uterine pathologies and endometrial polyps are the most frequent findings in asymptomatic postmenopausal women with an endometrium measuring >5mm. Conclusions: The results don’t justify the need for routine use of transvaginal ultrasound as a screening test for endometrial cancer as it is quite rare in asymptomatic postmenopausal women. When deciding how to manage imaging findings individual patient risk needs to be analyzed in order to avoid overtreatment.
Keywords: GDM, Fist trimester screening, PlGF, IL-6, OCN, Pregnancy, Glucose
Introduction
Transvaginal ultrasonography (TVS) is the most cost-effective first line test tool, which is used for the identification of symptomatic post-menopausal patients with a risk of endometrial cancer1,2. Those with an increased endometrial thickness at the first TVS examination, are characterized as high-risk patients. As a consequence, the next step for them is to be referred, in order to undergo further investigation and treatment.
Endometrial carcinoma is the most common cancer of the female genital tract in developed countries, and its clinical manifestation is postmenopausal bleeding in more than 95% of cases3,4. Guidelines recommend a cut-off value of 4 to 5mm by transvaginal ultrasonography (TVS), below which the probability of endometrial carcinoma is less than 1% for women with postmenopausal bleeding3. Nevertheless, the consequence of a thick endometrium, which is incidentally found in TVS examination of asymptomatic postmenopausal women, is not known yet5.
Most cases of endometrial cancer occur in women with vaginal bleeding6. This symptom is the presenting complaint in more than 90% of postmenopausal women with endometrial cancer, and it is associated with a 1–10% risk of endometrial cancer7,8. But a preclinical stage might exist, during which some cancers could be found prior to the manifestation of symptoms and thus exists the rationale for considering biopsy in a woman who is not experiencing vaginal bleeding. In addition, in some cases of atrophic cervix and stenosis malignancy does not present with bleeding until they have progressed beyond advanced stage of endometrial carcinoma. Endometrial hyperplasia with nuclear atypia is believed to be a precursor lesion of endometrial carcinoma.. Many studies until now have shown that the prevalence of coexisting carcinoma for women with atypical endometrial hyperplasia after an endometrial sampling, varied between 17% and 52%. Dordevic9, spoke about it and the frequency of coexisting endometrial carcinoma, and reported that it was significantly higher in complex atypical hyperplasia, in contrast to simple atypical hyperplasia cases. One recent data analysis conducted in European women, showed that endometrial cancer is increased and has an increasing rate in northern and western countries10.
In order to take the right decision following the measurement of endometrial thickness by transvaginal ultrasound in symptomatic postmenopausal women, various professional groups have recommended different endometrial thickness cut-off values. The Society of Gynaecologic Oncology and Society of Obstetricians and Gynaecologists of Canada recommend ≤5mm, the American College of Obstetricians and Gynaecologists (ACOG) committee recommends ≤4 mm11, and the National Clinical Guideline of the Scottish Intercollegiate Guidelines Network recommends ≤3 or ≤5mm to be used12, depending on whether the patient is using hormone replacement therapy (HRT) or not4. Nevertheless, most of the studies present a lack of precise estimations or have used less clinically meaningful measures of diagnostic accuracy in asymptomatic postmenopausal women. Their results are often conflicting and confusing. The measurement of endometrial thickness by ultrasound alone cannot rule in endometrial hyperplasia or carcinoma. On the contrary, if we use the best quality studies at a 5mm cut-off level measuring both layers, ultrasonography can be used to rule out endometrial hyperplasia or carcinoma with good certainty, in postmenopausal bleeding cases only, as it reduces the post-test probability of endometrial disease to 2.5%. The American College of Obstetricians and Gynecologists Committee Opinion No.440 states that a thickened endometrium in postmenopausal women needs not to trigger further evaluation in the absence of bleeding. They recommend an individualized approach based on woman’s characteristics and risk factors. But many of these women, and especially the obese ones, are already at high risk because of increased body mass index.11
It is more than evident that, higher quality primary accuracy studies using ideal reference standards and good-quality criteria to guide decision-making in asymptomatic postmenopausal women are needed13,14. The aim of the present review is to assess and compare the diagnostic efficiency of TVS for discrimination between benign and malignant endometrial conditions in postmenopausal women with thickened endometrium without any symptoms of bleeding. Moreover, the aim is to evaluate the cut off risk for endometrial cancer by transvaginal ultrasound measurement in women, who have entered menopause as a screening tool.
Materials and methods
Inclusion and exclusion criteria of studies
High quality cohorts, Randomized controlled trials (RCTs) and relevant systematic reviews/metanalysis written in English, were considered eligible for inclusion.
The inclusion and exclusion criteria, which were used, are the following:
Inclusion criteria:
- Articles written in the English Language
- Postmenopausal women, which defined as the absence of menstruation for at least 12 months after 40 years of age
- Any pathological cause of amenorrhea excluded.
- RCTs, Metanalysis, Systematic reviews, high quality cohort
Exclusion criteria:
- Vaginal bleeding
- Treatment with tamoxifen
- Hormone replacement therapy or anticoagulants
- Oncological disease
- Articles written in any language other than English
- Case reports, Editorials, Letters, Comments
- No access to full-text
Types of interventions
Studies were considered eligible for inclusion as long as a thick endometrium has been found during ultrasound examination of postmenopausal asymptomatic women, and then followed investigation of histology by hysterectomy, dilatation and curettage, hysteroscopy with biopsy, endometrial biopsy to reveal any type of pathology or malignancy in the endometrium.
Types of outcome measures
Primary outcomes
- Ultrasound endometrial thickness-defined as the measurement of endometrial thickness by transvaginal ultrasound in asymptomatic postmenopausal women.
Secondary outcomes
- Endometrial histological result-defined as the evaluation of endometrium by histology (hysterectomy, dilatation and curettage, hysteroscopy with biopsy, endometrial biopsy) or by cytology.
- Endometrial pathological lesions–discrimination between benign and malignant endometrial conditions in postmenopausal women with thickened endometrium.
- Symptomatic postmenopausal women-defined as the women one year after their last menstrual cycle, presenting with symptoms mostly endometrial bleeding.
- Asymptomatic postmenopausal women-defined as the women one year after their last menstrual cycle, presenting without symptoms.
Search methods for identification of studies
In order to identify all studies related to the systematic review question, a detailed search strategy that took into account all important aspects of the clinical question and an appropriate study design, was developed. Key words used were: asymptomatic postmenopausal women, atypical hyperplasia, endometrial cancer, transvaginal ultrasound, screening, endometrial thickening. Thus, eligible studies were identified by a predefined search strategy in electronic databases, hand searching, reference lists and contacting authors.
Electronic database searches
Our search strategy for evidence included 2 major medical databases for postmenopausal women without symptoms and with symptoms mainly due to postmenopausal bleeding, in order to correlate the two populations and understand the significance of endometrial thickness better. The medical databases used were PubMed (appendix) and Cochrane Database of Systematic Reviews (CDSR). The major motive for using these materials was their popularity, high scientific level and availability.
Selection of studies, data extraction and analysis
Two reviewers (AD and DB) independently assessed study characteristics and methodological details of included studies using data extraction forms. Differences in opinion were to be resolved by consensus and consultation of the third reviewer (DC). Where additional information on trial methodology or original trial data was required corresponding authors were contacted. Reminder correspondence was sent if a reply was not received within two weeks. When multiple publications on the same subject were encountered, then the largest relevant study was included. Specifically the following items were extracted by the studies: Study information, baseline characteristics of population (age, postmenopausal), endometrial thickness by ultrasound, outcome data (hyperplasia, endometrial polyp, malignancy) and study characteristics (cohort, RCT, systematic reviews, metanalysis).
Method of study quality assessment – Assessment of risk of bias in included studies
Risk of bias of each study was assessed by using the Cochrane Collaboration tool15 for assessing the risk of bias which covers: sequence generation, allocation concealment, blinding, incomplete outcome data, and selective outcome reporting. Based on the extracted information from each study each of the six domains was judged and rated as <high>, <low> or <unclear> risk. These judgements were performed independently by two reviewers and disagreements were resolved by discussion. Only studies with more than 70% <high> rate have been included to the final review.
Results
In order to evaluate normal endometrial thickness in asymptomatic postmenopausal women, the reviewers searched for studies that reported a mean endometrial thickness with a measure of variance and described a standardized approach to measurement of endometrial thickness by TVS. To assess the prevalence of (pre)malignant lesions of the endometrium in asymptomatic postmenopausal women, they included studies that reported on any form of endometrial verification in the total population of asymptomatic postmenopausal women not using HRT. To estimate the diagnostic accuracy of endometrial thickness for (pre)malignancy of the endometrium, they selected studies that reported on both endometrial thickness measurement and endometrial histological verification in asymptomatic postmenopausal women. The employed search strategy in data bases identified 419 articles. Then, manually excluded any duplicates, articles that did not provide the full text freely, and irrelevant articles by title or abstract, resulting in 154 full text available articles. Finally screening of the full text was conducted, concluding the search to 48 studies.

Figure 1. Prisma table
From these 5 cohorts and metanalysis for asymptomatic and 2 for symptomatic women, were found to be eligible according to inclusion criteria (PRISMA Figure 1). The 5 studies referring only to asymptomatic women that were finally included to the review had more than 70% <high> quality rate (Figure 2).
Design-Sample size
The reviewers searched and studied a total number of postmenopausal women equal to 143515, from which 127611 were the asymptomatic and 15904 were the symptomatic. Due to the inclusion and exclusion criteria, finally 31378 asymptomatic and 4686 symptomatic women were included. From all of them, histological examination revealed endometrial cancer 2212 (801 asymptomatic – 1411 symptomatic), endometrial polyps 832 (173 asymptomatic – 659 symptomatic) and 204 cases of hyperplasia, both types simplex and complex (169 asymptomatic – 35 symptomatic) (Table 1). Patient characteristics showed no significant differences with regard to age, age at menarche, age at menopause and BMI.
Analysis of the results in asymptomatic postmenopausal women with endometrial thickness
- The role of ET for endometrial pathology detection
The purpose of the retrospective cohort by Saatli B5 was to estimate the importance of endometrial sampling in postmenopausal women without symptoms like bleeding, who had endometrial thickness greater or equal to 5mm on transvaginal ultrasound measurement. The medical records of 12.643 women, were followed-up and were reviewed between January 2.000 and March 2009. Between these patients, a total of 530 women were discovered to have an endometrial thickness of 5mm or above without any symptom of vaginal bleeding and an endometrial sampling was performed for all of them. Out of total, of 530 the 289 (56%) biopsies were performed by Pipelle method, 174 (32%) of them by fractional curettage and only the rest 67 (12%) by hysteroscopy. The mean endometrial thickness was 8.7mm (range: 6–26). The number of patients with simple hyperplasia without atypia was 74 (13.9%), simple atypical hyperplasia 56 (10.5%) and atypical complex hyperplasia 9 (1.6%). There were only 5 (0.9%) cases of endometrial adenocarcinoma diagnosed, from which Pipelle method was used in 2 of them and fractional curettage was used in 3 of them for sampling of endometrium. Women, who presented endometrial adenocarcinoma, were under neither hormone replacement therapy, nor tamoxifen. The endometrial thickness of these women in TVS was 6mm in 2 women, 8mm in another two women and one had 11mm. Results showed only 5 (0.9%) endometrial adenocarcinomas among 530 women with endometrial thickness 5mm or above without any symptom of vaginal bleeding.
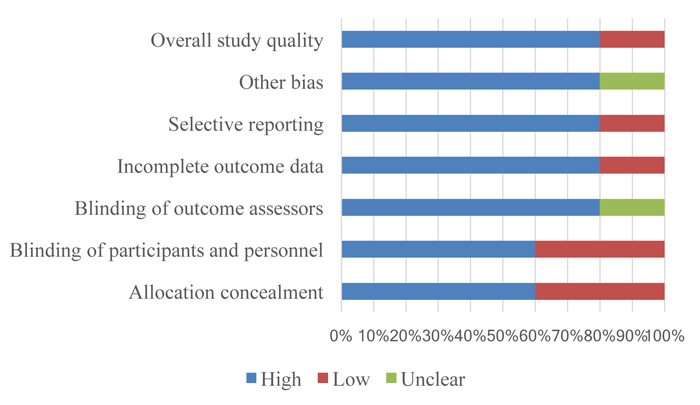
Figure 2. Type of studies included to the review and quality assessment
- Capacity of ET measurement to diagnose endometrial pathology
The purpose of the metanalysis by Breijer MC3, was to define the normal endometrial thickness measured by TVS, the risk of serious endometrial pathology and the sensitivity and specificity of endometrial thickness measurement by TVS for diagnosing premalignant and malignant endometrial disease in asymptomatic postmenopausal women. In total, 11100 women were included from thirty-two studies. They concluded that the risk of malignancy in a woman below the threshold of 4mm is extremely low, and the risk of malignancy above it varies between 2.2 and 9.3%.
Nevertheless, the significance of the thickness of the endometrium beyond 4 mm is not the same as for symptomatic postmenopausal women, and extrapolating guidelines from postmenopausal bleeding to asymptomatic population is not valid in view of the low overall disease prevalence and poor performance of TVS in detecting serious endometrial disease at all cut-offs.
- Malignancy risk for asymptomatic with raised ET
In the following retrospective cohort Famuyide A16, involved 154 postmenopausal women, who attended to the clinic in order to have hysteroscopy because of endometrial measurement of 4mm on transvaginal ultrasound, including women who had possibly endometrial polyp, and did not have any other symptoms, like For all the 154 participants, the range of the measurement of the endometrium was 4.2 to 28mm. Endometrial biopsies (EMBs) were done in 109 patients, and the result was negative for cancer or an atypical endometrium. Authors found that endometrial carcinoma and atypia do occur in almost 1% of women with asymptomatic endometrial thickening and in 2.7% of women who underwent removal of the endometrial polyps. In both groups, endometrial measurements were ≥17mm. EMBs performed in the office settings were not conclusive, and polypectomies was required for final diagnosis.
In conclusion, when office flexible hysteroscopy is used, endometrial polyps are the most frequent findings in asymptomatic women with a thickened endometrium. Carcinoma will be found though in a significant number of patients who undergo polypectomy. So, there is a need for a close estimation of the uterus for structural or focal lesions, and when endometrial polyps or focal lesions are diagnosed, it is proposed to be removed even in the absence of vaginal bleeding.
- When should asymptomatic ET promptbiopsy?
Smith-Bindman6, suggested in their metanalysis a cut-off value of 11mm for endometrial biopsy for asymptomatic postmenopausal women, whereby the risk of malignancy would be approximately equal to that of a symptomatic woman with an ET of 5mm. The aim of this analysis was to calculate an endometrial thickness in asymptomatic women that would match the malignancy risk in women with bleeding and an endometrial measurement of ≤5mm.
According to the conclusions of Smith-Bindman6, in a postmenopausal woman with vaginal bleeding, the risk of cancer is approximately 7.3% if her endometrium is thick (>5mm) and <0.07% if her endometrium is thin (≤5mm). In postmenopausal women without vaginal bleeding, the risk of cancer is approximately 6.7% if the endometrium is thick (>11mm) and 0.002% if the endometrium is thin (≤11mm). This means that, if the endometrium measures ≤11mm in a postmenopausal woman without vaginal bleeding, endometrial biopsy is not necessary as the risk of cancer is low. But each patient should be valued individually below 11mm.
The risk of endometrial cancer is approximately 0.07% if the endometrium is thin (≤5mm) and 7.3% if it is thick (>5mm) in a postmenopausal woman with vaginal bleeding. Controversially in a postmenopausal woman without vaginal bleeding, the risk of cancer is almost 0.002% if her endometrium is thin (≤11mm) and 6.7% if the endometrium is thick (>11mm). In a woman without bleeding, if the definition of a normal endometrial thickness is lowered from 11 to 7mm (so that a measurement of 8mm or greater would be considered abnormal), the cancer risk in a woman with a ‘thick endometrium’ is only 2.1%. By lowering the cut-off from 11 to 7mm, the cancer detection rate would increase slightly (from 87% to 95%) but the false- positive rate would quadruple (from 0.25% to 0.90%). In conclusion 15% of cancers occur in women without vaginal bleeding. As a woman’s age increases, her risk of cancer increases at each endometrial thickness measurement. Using the 11mm threshold, the risk of cancer increased from 4.1% at age 50 years to 9.3% at age 79 years. Varying the other estimates used in the decision analysis within possible thickness ranges had no substantial effect on the results.
- Accuracy of ET and appropriateness of performed hysteroscopies
Giannella4, tried to estimate the diagnostic accuracy of endometrial thickness for the detection of all intra-uterine pathology among asymptomatic postmenopausal women. She included in her prospective study 268 asymptomatic postmenopausal women with endometrial thickness 4 mm who were referred for diagnostic hysteroscopy.
The results of the study showed that no endometrial thickness cut-off values had optimal diagnostic accuracy [positive likelihood ratio (LR+) >10 and negative likelihood ratio (LR-)<0.1]. The greatest endometrial thickness cut-off value for the detection of all intra-uterine pathologies was 8 mm (LR+ 10.05 and LR- 0.22). An endometrial thickness cut-off value of 10 mm did not miss any endometrial malignacy. The success rate of diagnostic hysteroscopy was 89%, but 97% of these revealed a benign intra-uterine pathology. The diagnostic accuracy of hysteroscopy was optimal for all intra-uterine pathologies, except endometrial hyperplasia (LR 0.52). Final conclusion was that by using an endometrial thickness cut-off value of 4 mm, only 3% of hysteroscopies, could detect pre-malignant or malignant les lesions. Even though endometrial thickness did not show optimal diagnostic accuracy, using the best cut-off value (8 mm) it may decrease the number of false-positive results. In the end, there were no cases of endometrial malignancy, which were diagnosed in asymptomatic postmenopausal women with endometrial thickness <10 mm.
Discussion
In women with postmenopausal bleeding, the significance of TVS has been thoroughly studied. It is found that an endometrial measurement of 4 to 5mm or less has a negative predictive value for endometrial cancer of 99.4% or greater11. The interpretation and clinical management of an incidentally noted thick endometrium though has not been standardized and the exact threshold for endometrial measurement among asymptomatic postmenopausal women is still unclear.
Our study tried to systematically review the literature in order to estimate the results of histological examination of the endometrium in postmenopausal women without vaginal bleeding, who had thickened endometrium on TVS during follow-up in a menopause clinic. Endometrial cancer is usually associated with vaginal bleeding and the risk of cancer is very low in women without bleeding 3. Nowadays, screening for endometrial cancer is only recommended in women with Lynch syndrome, whose lifetime endometrial cancer risk is 40–60%17 But as the life expectancy increases, there is a change in this understanding as well as the case with other solid organ cancers. In the end there is no consensus to which is the optimal endometrial thickness that should trigger the appropriate investigations in order to rule out endometrial malignancy.
Several investigators have advised that even an endometrial measurement, by less than 8mm, should prompt biopsy in asymptomatic women18,19. This recommendation to biopsy a woman with an incidentally found endometrial measurement of 8mm does not take into account the low risk of endometrial cancer between women without vaginal bleeding.14,15 Intrauterine pathologies in postmenopausal women without symptoms are quiet common up to 13%19 and appear mostly as polyps. In these cases no treatment is actually needed. In an another study based on ultrasound screening of postmenopausal women without bleeding, a cut-off of 5mm had a positive predictive value of 1.4%, and for 10mm, the positive predictive value was 4.5% and the negative predictive value was 99.9% for both cut-offs20. Authors concluded that polyps of endometrium are the most frequently encountered lesions in asymptomatic women. In contrast, the endometrial cancer presents with uterine bleeding in more than 90% of cases, and in 75% of women is at an early stage. Gerber21, showed there was no prognostic benefit gained examining women without bleeding but with increased ET, compared to women who are examined within eight weeks of the onset of vaginal bleeding. Thus, risk of over treating benign pathology is unacceptably high. In a cohort study by Ribeiro et al. 2007, no cases of cancer or hyperplasia were detected with an ET <8mm even if this was expanded to include symptomatic women with vaginal bleeding (n=457).
Using the data of our review analysis, and in comparison with the cut off that is widely accepted in women with bleeding, it seems that an endometrial thickness measurement of ≥11mm gives a reasonable safe limit to perform biopsy in postmenopausal women without vaginal bleeding, as the risk is 6.7% which is comparable to the 5mm risk of 5% for symptomatic postmenopausal women6. There is no doubt that we have to estimate and to take into account individual patient risk factors when deciding how to manage imaging findings. A woman with known risk factors for endometrial cancer like diabetes, which increases the risk of endometrial cancer three-fold, or obesity, which increases the risk of cancer 10-fold, or the use of unopposed estrogen or tamoxifen, which increases the risk two-fold or age >70 years, will have a higher risk of cancer than one without such risk factors, even with the same endometrial thickness measurement6. In addition, till now we have to consider only endometrial thickness, and no other components of endometrial appearance such as homogeneity, nodularity and Doppler flow characteristics. There are insufficient data on these characteristics to determine how they should be used in screening for endometrial cancer6. A large cohort study of postmenopausal women provided from the United Kingdom Collaborative Trial of Ovarian Cancer Screening study22, was published and involved 37038 women after random assignment. With an endometrial thickness cut-off of 5mm, sensitivity was 80.5% and specificity was 85.7% for endometrial cancer or atypical hyperplasia. According to the results in this study they have detected 5 cases of endometrial adenocarcinoma, and one more endometrial adenocarcinoma was detected in the final histopathology of women undergoing hysterectomy for atypical hyperplasia, between 530 postmenopausal asymptomatic women having an endometrial stripe equal to 5mm or more. Dueholm13 advocated that a threshold of ≤4mm should be normal in postmenopausal women with vaginal bleeding, and ≥5mm should be thought as abnormal. The danger of cancer is approximately 4.6% in postmenopausal women with vaginal bleeding if the endometrium measures ≥5mm. From the other side, a threshold of 10mm (i.e. ≤10mm is considered normal) in women without vaginal bleeding and is associated with a similar low cancer risk.
In our review we have tried by applying strict criteria of inclusion, to achieve the highest possible quality assessment of evidence. The findings of this review, describe normative values for endometrial thickness, determine serious disease prevalence and estimate diagnostic accuracy at various TVS thresholds in non- bleeding postmenopausal population. The main limitation of our study is that although a significant number of asymptomatic post-menopausal women have been included to the review, because of the low prevalence of the disease in our study group, most of the studies had insufficient data with a wide range of sensitivity and specificity, thus making the estimate of the optimal threshold of endometrial thickness not possible.
In conclusion, it is more than obvious that the threshold of 4–5mm endometrial thickness, which is used in symptomatic postmenopausal women, may not be also used as so in postmenopausal women without bleeding as the risk of overtreatment is imminent. The results of our study don’t justify the need for routine use of transvaginal ultrasound as a screening test for endometrial cancer as the incidence of this pathology is extremely low in the group of asymptomatic postmenopausal women. We should though consider the rising incidence of endometrial cancer, and the requirement for more and larger prospective trials with surrogate criteria for thickened endometrial stripe in postmenopausal women in TVS for both symptomatic and asymptomatic women.
Acknowledgements
The authors acknowledge the helpful comments of the authors of included trials who supplied additional information or data in the previous and current review.
Contribution of authors
Angelos Daniilidis conceptualized the protocol and the review primarily, and carried out the search, selection of trials and risk of bias assessment as a first reviewer and first author in the first version of the review and as a second reviewer in the current update.
Dimitris Balaouras conducted the current update by performing the search and selection of trials, risk of bias assessment as a first reviewer and author.
Dimitris Chitzios was available to resolve discrepancies for differences of opinion between the other authors and added content expertise to the discussion and conclusions during the first and updated version of this review.
Chrisanthi Sardeli conducted proof reading of the primary protocol and carried out comments to the results and discussion section.
Apostolos Mamopoulos conducted proof reading of the primary protocol and carried out comments to the results and discussion section.
Efstratios Assimakopoulos was the main reviewer of the all structure and presentation of evidence, by giving specific guidedance and rules to the outcome of this systematic review.
Appendix for the Search strategy in Pubmed
#1. Postmenopause [MeSH]
#2. Postmenopaus*
#3. #1 OR #2
#4. Asymptomatic[MeSH Terms]
#5. # 3 AND # 4
#6. Ultrasound [MeSH]
#7. Ultrasonograph* [tiab]
#8. Transvaginal
#9. #6 OR #7
#10. #9 AND #8
#11. Endometrium [MeSH]
#12. Endometrial thickness
#13. #11 AND #12
#14. Endometr* cancer
#15. Endometr* malignanc*
#16. Endometr* neopl*
#17. #14 OR #15 OR #16
#18. Endometr* hyperplasia
#19. Endometr* polyps
#20. #18 OR # 19
#21. #20 OR #17
#22. #5 AND # 21
#23. # 22 AND # 10
(((((((endometr* AND hyperplasia) OR endometr* AND polyps)) OR (((endometr* AND can- cer) OR endometr* AND malignanc*) OR endometr* AND neopl*))) AND ((((postmenopaus*) OR postmenopause[MeSH Terms])) OR asymptomatic[MeSH Terms]))) AND ((((transvaginal) AND ultrasound[MeSH Terms])) OR ((transvaginal) AND ultrasonogra*))
References
2. Smith-Bindman R, Kerlikowske K, Feldstein VA, Subak L, Scheidler J, Segal M, et al. Endovaginal ultrasound to exclude endometrial cancer and other endometrial abnormalities. Journal of American Medical Association 1998; 280: 1510-7.
3. Breijer MC, Peeters JAH, Opmeer BC, Clark TJ, Verheijen RHM, Mol BWJ et al. Capacity of endometrial thickness measurement to diagnose endometrial carcinoma in asymptomatic postmenopausal women: a systematic review and meta-analysis. Ultrasound in Obstetrics and Gynecology 2012; 40: 621–9.
4. Giannella L, Mfuta K, Setti T, Boselli F, Bergamini E, Cerami LB. Diagnostic accuracy of endometrial thickness for the detection of intra-uterine pathologies and appropriateness of performed hysteroscopies among asymptomatic postmenopausal women. European Journal of Obstetrics Gynecology and Reproductive Biology 2014;177: 29–33.
5. Saatli B, Yildirim N. Olgan S, Koyuncuoglu M, Emekci O, Saygili U. The role of endometrial thickness for detecting endometrial pathologies in asymptomatic postmenopausal women. Australian and New Zealand Journal of Obstetrics and Gynaecology 2014; 54:36–40.
6. Smith-Bindman R, Weiss E and Feldstein V. How thick is too thick? When endometrial thickness should prompt biopsy in postmenopausal women without vaginal bleeding. Ultrasound in Obstetrics and Gynecology 2004; 24: 558–565.
7. Goldstein RB, Bree RL, Benson CB, Benacerraf BR, Bloss JD, Carlos R et al. Evaluation of the woman with postmenopausal bleeding: Society of Radiologists in Ultrasound-Sponsored Consensus Conference statement. Journal of Ultrasound in Medicine 2001; 20:1025–1036.
8. Rose PG. Endometrial carcinoma. New England Journal of Medicine 1996; 335:640–9.
9. Dordević B, Stanojević Z, Zivković V, Lalosević D, Gligorijević J, Krstić M. Preoperative and postoperative histopathological findings in patients with endometrial hyperplasia. Medicinski Pregled 2007; 60: 372–6.
10. Bray F, Dos Santos Silva I, Moller H, Weiderpass E. Endometrial cancer incidence trends in Europe: underlying determinants and prospects for prevention. Cancer Epidemiology and Biomarkers Prevalence 2005; 14: 1132–1142.
11. REF American College of Obstetricians and Gynecologists. The role of transvaginal ultrasonography in the evaluation of postmenopausal bleeding. ACOG Committee Opinion No. 440. Obstetrics and Gynecology 2009;114: 409–411.
12. Scottish Intercollegiate Guidelines Network. Investigation of postmenopausal bleeding. Scottish Intercollegiate Guidelines Network, Royal College of Physicians 2002.
13. Gupta JK, Chien PFW, Voit D, Clark TJ and Khan KS. Ultrasonographic endometrial thickness for diagnosing endometrial pathology in women with postmenopausal bleeding: a meta-analysis. Acta Obstetrica et Gynecologica Scandinavica 2002; 81:799–816.
14. Dueholm M, Holm JW, Rydbjerg S, Hansen ES and Ørtoft G . Two and three-dimensional transvaginal ultrasound with power Doppler angiography and gel infusion sonography for diagnosis of endometrial malignancy. Ultrasound in Obstetrics and Gynecology 2015; 45(6):734-743.
15. Higgins JPT, Altman DG. Chapter 8: Assessing risk of bias in included 11 studies. In: Higgins JPT, Green S, eds., Cochrane handbook for systematic reviews of interventions version 5.0.0. The Cochrane Collaboration. Available: http://www.cochrane-handbook.
16. Famuyide A, Breitkopf D, Hopkins M, Laughlin-Tommaso S. Asymptomatic Thickened Endometrium in Postmenopausal Women: Malignancy Risk. Journal of Minimally Invasive Gynecology 2014; 21(5): 782-786.
17. Wang Y, Wang Y, Li J, Cragun J, Hatch K, Chambers S et al. Lynch syndrome related endometrial cancer: clinical significance beyond the endometrium. Journal of Hematology and Oncology 2013; 6:22.
18. Disaia P, Creasman W . Clinical Gynecologic Oncology (6th edn). Mosby-Year Book: St Louis, MO 2002.
19. Dreisler E, Sorensen SS, Ibsen PH and Lose G. Value of endometrial thickness measurement for diagnosing focal intrauterine pathology in women without abnormal uterine bleeding. Ultrasound in Obstetrics and Gynecology 2009; 33: 344–348.
20. Jacobs I, Gentry-Maharaj A, Burnell M, Manchanda R, Singh N, Sharma A et al. Sensitivity of transvaginal ultrasound screening for endometrial cancer in postmenopausal women: a casecontrol study within the UKCTOCS cohort. Lancet Oncology 2011; 12:38–48.
21. Gerber B, Krause A, Müller H, Reimer T, Külz T, Kundt G et al. Ultrasonographic detection of asymptomatic endometrial cancer in postmenopausal patients offers no prognostic advantage over symptomatic disease discovered by uterine bleeding. European Journal of Cancer 2001; 37: 64–71.
22. Menon U, Gentry-Maharaj A, Hallett R, Ryan A, Burnell M, Sharma A et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS). Lancet Oncology 2009; 10:327–340.