Research
HJOG 2022, 21 (1), 25-34 | doi: 10.33574/hjog.0403
Panagoula Katzeni1, Eleftherios Zachariou2, Dimitrios Papageorgiou2, Georgios Daskalakis2, Vasilios Pergialiotis2
1Unit of Obstetrics and Gynecology, General Hospital of Argolis, Argolis, Greece
21st department of Obstetrics and Gynecology, Unit of Gynecologic Oncology, Alexandra Hospital, National and Kapodistrian University of Athens, Greece
Correspondence: Vasilios Pergialiotis, MD, MSc, PhD, 6, Danaidon Str. Halandri 15232 – Greece, e-mail: pergialiotis@yahoo.com,
Abstract
Introduction: Breastfeeding is the unparalleled way to provide infants the ideal nutrients they need for their healthy growth. The World Health Organization (WHO) recommends exclusive breastfeeding until 6 months old, starting within 1 hour of birth. All infants should start receiving foods in addition to breast milk from 6 months onwards, while breastfeeding continues until 2 years old or more.
Purpose: The purpose of this study is to investigate those factors that may influence the onset of breastfeeding in the first few days after birth and during the hospitalization in the maternity ward, as well as the establishment of breastfeeding 6 weeks after birth, along with studying the weight of the newborn.
Material and Method: This was a prospective study with a convenience sample taking place in the General Hospital of Argolis and the Elena Venizelou maternity hospital in Athens. In the presented pilot study 75 women that delivered at full term completed the questionnaire. We chose to exclude women that delivered during the preterm period as well as those that delivered twins as these factors independently affect the possibility of discontinuing breastfeeding. A self-report questionnaire with closed and open-ended questions was used and was completed in two phases.
Results: Overall, 75 women completed the questionnaire. Of those 3 women delivered within the early term period (37+0 – 38+6 weeks). The majority of women (74.67%) initiated breastfeeding within 2 hours from delivery. Rooming in was allowed within the first hour in a large proportion of participants (62.67%). Breastfeeding difficulties were encountered in approximately half of participants and the predominant reason was some form of breast pathology. Twenty-two mothers (29.3%) discontinued breastfeeding within the study period. Early rooming in significantly increased the possibility of continuing breastfeeding after the first month. Of all the factors that were investigated during the puerperal period only the amount of formula meals significantly affected the rates of continuous breastfeeding.
Conclusion: Early rooming-in significantly increases breastfeeding practices. Unstructured educational activities from healthcare providers and accompanying brochures do not seem to enhance breastfeeding duration, indicating the need for adoption of specific programs that will be tested in forthcoming studies.
Keywords: Breastfeeding, lactation, Greece, rural, urban
Introduction
Breastfeeding, is considered to one of the most determining factors for the physical and neurological development of the newborn and the infant. It provides infants with the active and nutritious ingredients to grow in the first months of life and continues to meet their nutritional needs, even when complementary feeding is started. Promotes cognitive development, protects against chronic and infectious diseases, reduces infant mortality and helps in faster recovery during illness. In the Greek population the duration of breastfeeding has been directly related to cognitive, language and motor development at 18 months of age1. It also contributes to the health and well-being of mothers by reducing the risk of breast and ovarian cancer and creating a time gap between births. The World Health Organization (WHO) recommends exclusive breastfeeding for the first 6 months of an infant’s life followed by partial breastfeeding until the age of 2 or more.
The value of breastfeeding is well recognized in low- and middle-income countries, but in high-income countries there seems to be less consensus on its value. However, in low-income countries only 37% of children under 6 months are exclusively breastfed. With only a few exceptions, the duration of breastfeeding in high-income countries is even shorter than in those with poorer resources2.
Worldwide, the rates of exclusive breastfeeding for children 0-5 months are extremely low reaching only 41%3. Approximately 40% of newborns receive breastfeeding within the first hour of life. Less than 75% continue to breastfeed until the 12th -15th month. Despite the WHO recommendation for continued breastfeeding until the age of 2 years, less than half, aged 20-23 months, benefit from it4,5. In Greece several educational activities have been established in the past indicating that a structured midwifery breastfeeding education may enhance the rates of acceptability of breastfeeding5. The last year, with the emerge of COVID-19 rates of exclusive breastfeeding fell in parturient that were diagnosed with the disease to an extremely low percentage of 7.2%6.
The aim of our study was to investigate those factors that affect the onset and consolidation of breastfeeding.
Materials and methods
We designed a prospective cohort study that assessed the impact of maternal, paternal and neonatal characteristics on breastfeeding duration. The study was approved by the institutional review board of Attikon University Hospital of the National and Kapodistrian University of Athens. The study was conducted in 2 hospitals: 1) the General Hospital of Argolis (a suburban hospital that serves a suburban and urban sample of the Greek population) and, b) Elena Venizelou Maternity hospital (an urban tertiary referral center established in Athens). In the presented pilot study 75 women that delivered at full term completed the questionnaire. We chose to exclude women that delivered during the preterm period as well as those that delivered twins as these factors independently affect the possibility of discontinuing breastfeeding. A self-report questionnaire with closed and open-ended questions was used and was completed in two phases. Initially, the questionnaire was completed on the day of discharge and the women were again interviewed, by telephone or e-mail, during the 40th day of the puerperium.
Statistical analysis was performed in IBM SPSS (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). The normality of distribution was evaluated using the Kolmogorov Smirnov test and graphical methods. Univariate analyses were performed to evaluate the impact of health worker characteristics on the likelihood of suggesting the vaccination in pregnant women as well as women that wish to conceive naturally or with assisted reproduction.
Results
Overall, 75 women completed the questionnaire. Of those 3 women delivered within the early term period (37+0 = 38+6 weeks). Employment, educational and other relevant parental characteristics are briefly presented in Table 1. Of note, however, none of the 2 mothers that completed only the elementary school continued breastfeeding, while the lowest rate of discontinuation of breastfeeding (1/6, 16.6%) was observed among mothers with postgraduate studies. Also 3 of the 5 mothers who lived on an island (60%) stopped breastfeeding. The predominant reasons for continuation of breastfeeding were: i) perception of benefit for the offspring (92%), ii) perception of enhanced maternal-neonatal bonding (49.3%), iii) economic reasons (13.3%) and iv) perception of positive influence of breastfeeding on maternal health (32.0%).
Delivery characteristics and data relevant to the reason of discontinuation of breastfeeding are summarized in Table 2. The majority of women (74.67%) initiated breastfeeding within 2 hours from delivery. Rooming in was allowed within the first hour in a large proportion of participants (62.67%). Breastfeeding difficulties were encountered in approximately half of participants and the predominant reason was some form of breast pathology (mainly erosions of the nipple) (Table 3). Approximately 90% of women were informed for the benefits of breastfeeding either by accompanying leaflets or from healthcare providers (midwifes, nurses and physicians). The majority of women used formula as an adjunct to breastfeeding whereas 5 women opted out of breastfeeding. Twenty-two mothers (29.3%) discontinued breastfeeding within the study period.
Concerning parental characteristics, inferential analysis revealed that none of them significantly affected the risk of discontinuation of breastfeeding (Table 4). On the other hand, early rooming in significantly increased the possibility of continuing breastfeeding after the first month (Table 5). Of all the examined maternal and neonatal pathologies that could affect breastfeeding rates, only the diagnosis of respiratory distress syndrome in the neonate was close to being a significant predictor of discontinuation of breastfeeding; however, the limited population size of our study did not allow for the result to reach the predetermined level of statistical significance.
Of all the factors that were investigated during the puerperal period only the amount of formula meals significantly affected the rates of continuous breastfeeding (Table 6). Prior breastfeeding was increased in women that continued to breastfeed in our study, however, the sample size did not allow this variable to reach the required statistical significance. Neither the interval from delivery to start of breastfeeding nor the timing of rooming in significantly affected the odds of continuing breastfeeding after the study period (Figure 1). Of note, the receipt of information from healthcare providers and relevant brochures did not affect maternal choice of continuing breastfeeding, despite the fact that 25% of participants was not informed about the benefits of breastfeeding prior to the onset of the study.
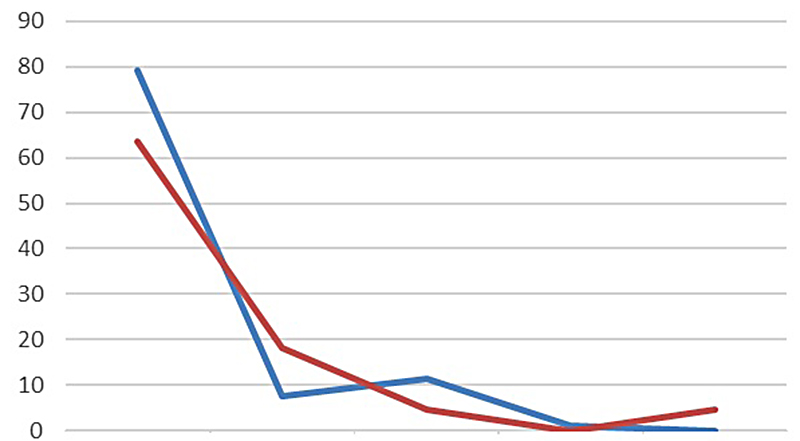
Figure 1. Breastfeeding rates per timing of initation of breastfeeding.
Discussion
The present study showed that rooming-in significantly influences maternal decision to breastfeed. Moreover, the level of education seems to be a potentially related factor, despite the fact that the appropriate level of statistical significance was not reached. Indeed, the level of basic education is important in the proportion of mothers who breastfeed in the first hour after birth. Women with a level of education above high school have a higher intention to breastfeed, as a higher level of education makes women more able to seek relevant information on optimal infant feeding and, more likely, to breastfeed their infant7. Furthermore, several studies show a direct correlation between the level of education and the frequency of initiation and continuation of breastfeeding8,9.
Likely, efforts in recent decades to promote breastfeeding and messages about the clear benefits of breast milk have influenced those women with the highest levels of education more easily. These women are also more likely to have higher socioeconomic status and better jobs, which may let them continue breastfeeding for longer8,10. Also, mothers who are knowledgeable about the benefits of breast milk for the infant and her health are positive towards breastfeeding11,12.
There is no consensus on the influence of sociodemographic factors on the initiation and duration of breastfeeding. Maternal employment, cesarean section, and hospital admission are risk factors for early discontinuation of breastfeeding. However, there is no consensus on the effect of age, number of deliveries, and education13-21. In the present study, the small number of women probably did not allow statistically significant conclusions to emerge concerning these variables, except for education. Therefore, the effect of maternal education changes with circumstances, and its influence does not remain constant over time. This has two important implications: First, we need to consider the level of education. Second, the social environment should be considered as it may shape the aforementioned factors’ influence12,22.
As far as the number of children is concerned, the results of the surveys are rather contradictory. In primiparous women, prevention for breastfeeding is associated with prenatal care by a health professional, rather than with performing or not performing a cesarean section when the mother has contact with immediately after birth (rooming-in). The successful breastfeeding experience of the previous child constitutes a positive precedent for the mother to breastfeed her new child for longer and in an exclusive way19,22,23. The woman’s decision is strongly influenced by the family’s positive experiences with breastfeeding. Past experiences of family and friends and cultural values are also factors that influence breastfeeding initiation and duration24.
Breastfeeding is the exclusive role of women, but health professionals make a significant contribution to the success or failure of breastfeeding. In terms of health services, hospitals should implement policies that support breastfeeding, paying particular attention to limiting infant supplementation and extending professional support during hospitalization and the first weeks after birth, even though home care10,12,20.
According to UNICEF, global BF rates have stagnated since 1990, with only 36% of children under six months of age being exclusively breastfed worldwide in 2012.24 In the study by Yilmaz et al, the rate of early initiation of breastfeeding was 60.1%22. This rate is considered to be in the ‘good’ group according to the WHO classification [poor (0-29%), moderate (30-49%), good (50-89%) and very good (90-100%)24. The percentages were similar in the present study. The present study results compared to UNICEF can be explained by the fact that the clinics were located in an urban area serving a relatively better income group that has a higher rate of antenatal care and breastfeeding education than other areas of our country.
The effect of maternal education on increasing breastfeeding rates has been demonstrated in several studies19,22. The study by Yilmaz et al. found that antenatal education on breastfeeding was the most important predictor of breastfeeding duration22. One of the most important reasons for the early discontinuation of breastfeeding is insufficient knowledge of mothers about the importance of breast milk and breastfeeding techniques. Successful MT starts when the mother thinks she is going to breastfeed her baby and believes she can achieve it. The education is expected to increase mothers’ confidence.
A randomized controlled trial (RCT) (which included 176 mothers of infants) conducted in Russia showed that rooming-in significantly increased the rate of exclusive breastfeeding at discharge (4th day postpartum). The study included mother-infant pairs only after normal delivery and did not report whether there were any events such as infections. However, there is insufficient evidence to conclude the effects of this on breastfeeding up to six months26. Another non-randomized study found a higher breastfeeding rate at four months for primiparous but not multi-birth women who received rooming-in27.
Study limitations
This study is subject to certain limitations. A self-report questionnaire was used, which may have led to over-or underestimated practices and duration of MTH, as the study included a researcher’s partner for the Athens hospital. However, sufficient time has been allocated to all women to avoid hasty responses. Also, despite the prospective nature of the study, the reassessment was limited to 40 days (postpartum period) and was related to specific parameters, which prevented the identification of causal relationships of knowledge, and attitudes towards MTH. However, one of the two hospitals where the study was conducted was located in an urban area and the study is important for highlighting the effectiveness of baby-friendly hospital practices, while the other was located in a semi-urban area, and the study sample can be considered to be dimensionally reflective of the profile of mothers in the country, however, the convenience sample of women further limits the safe generalization of the study’s conclusions. Larger prospective studies (spanning a longer period and including a larger number of women) are needed to clarify the issues related to factors affecting MTH, as well as the initiatives that need to be taken to maintain and increase these rates in our country.
Conclusion
This study, despite its limitations, showed that breastfeeding culture and midwifery practices can significantly influence the establishment of exclusive breastfeeding in the first months of a newborn’s life. This effect is mainly observed in women of higher educational status. It remains unknown whether women with basic educational status may actually benefit from information available in brochures or communicated by healthcare professionals; however, structured plans are needed to promote the benefits of practicing breastfeeding. Although mothers largely perceive that breastfeeding is best for baby’s health and that it promotes mother-child bonding, the rate of exclusive breastfeeding in the second month was 50.7%, with complete cessation of breastfeeding occurring in one-third of mothers. Regular rooming-in and the mothers’ breastfeeding history favor the establishment of breastfeeding, while the systematic introduction of artificial milk in the infant’s diet and the mother’s low educational level discourage it. All of the above factors can be modified by appropriate information and education of the mother and her environment already during the prenatal period, while at the same time ensuring the correct application of midwifery practices. And herein lies the value of cooperation between the gynecologist and the midwife and the expectant mother, as well as the mother’s preparation courses during pregnancy. Indeed, during the courses in psycho prophylaxis, the expectant mother becomes familiar with the practices of lactation, fears and prejudices are dispelled and she is prepared for the difficult period of childbirth and postpartum. Although breastfeeding is a natural act,
Disclosure
The authors report no conflict of interest.
Funding
None
References
1. Leventakou V, Roumeliotaki T, Koutra K, Vassilaki M, Mantzouranis E, Bitsios P, Kogevinas M, Chatzi L. Breastfeeding duration and cognitive, language and motor development at 18 months of age: Rhea mother-child cohort in Crete, Greece. J Epidemiol Community Health. 2015;69:232-9.
2. Cai X, Wardlaw T, Brown DW. Global trends in exclusive breastfeeding. Int Breastfeed J. 2012; 7:12.
3. World Health Organization, United Nations Children’s Fund. Global breastfeeding scorecard, 2019: increasing commitment to breastfeeding through funding and improved policies and programmes. Geneva: World Health Organization; 2019. Contract No.: WHO/NMH/NHD/19.22
4. World Health Organization. (2014). Comprehensive implementation plan on maternal, infant and young child nutrition. World Health Organization. https://apps.who.int/iris/handle/10665/113048
5. Truva T, Valasoulis G, Pouliakis A, Gkorezi-Ntavela I, Pappa D, Bargiota A, Garas A, Grivea I, Daponte A. The Effect of a Structured Individualized Educational Intervention on Breastfeeding Rates in Greek Women. Int J Environ Res Public Health. 2021 Oct 28;18:11359.
6. Tigka M, Metallinou D, Nanou C, Iliodromiti Z, Lykeridou K. Frequency and Determinants of Breastfeeding in Greece: A Prospective Cohort Study during the COVID-19 Pandemic. Children (Basel). 2022 Jan 2;9:43.
7. Acharya P, Khanal V. The effect of mother’s educational status on early initiation of breastfeeding: further analysis of three consecutive Nepal Demographic and Health Surveys. BMC Public Health. 2015; 15:1069.
8. Colodro-Conde L, Sánchez-Romera JF, Tornero-Gómez MJ, et al. Relationship between level of education and breastfeeding duration depends on social context: breastfeeding trends over a 40-year period in Spain. J Hum Lact. 2011; 27:272-278.
9. Ramiro Gonzáleza MD, Ortiz Marrónb H, Ca˜nedo-Argüellesc CA, Esparza Olcinad MJ, Cortés Ricoe O, Terol Claramontef M, Ordobás Gavínb M. Prevalence of breastfeeding and factors associated with the start and duration of exclusive breastfeeding in the Community of Madrid among participants in the ELOIN. An Pediatr. 2018; 89:32-43.
10. Πολυτάρχου Α. Συχνότητα και διάρκεια μητρικού θηλασμού –παράγοντες προδιαθεσιακοι για πρώιμη διακοπή του. Μεταπτυχιακή διπλωματική εργασία. ΕΚΠΑ-ΤΕΙ Αθήνας, 2013.
11. Shiva F, Nasiri M. A study of feeding patterns in young infants. J Trop Pediatr. 2003; 49:89–92.
12. World Health Organization, UNICEF. Increasing commitment to breastfeeding through funding and improved policies and programmes: Global breastfeeding score card 2019.
13. Brown CR, Dodds L, Legge A, Bryanton J, Semenic S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Health. 2014; 105:e179-185.
14. Kambale MJ. Social determinants of breastfeeding in Italy. Afr Health Sci. 2011; 11:508–517.
15. Kimani-Murage EW, Madise NJ, Fotso JC, et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health. 2011; 11:396.
16. Al-Sahab B, Lanes A, Feldman M, et al. Prevalence and pre¬dictors of 6-month exclusive breastfeeding among Canadian women: a national survey. BMC Pediatrics. 2010; 10:20.
17. Pérez-Ríos N, Ramos-Valencia G, Ortiz AP. Caesarean delivery as a barrier for breastfeeding initiation: The Puerto Rican experience. J Hum Lact. 2008; 24:293–302.
18. Cohen SS, Alexander DD, Krebs NF, et al. Factors Associated with Breastfeeding Initiation and Continuation: A Meta-Analysis. J Pediatr. 2018; 203:190-196.e21.
19. Tavoulari EF, Benetou V, Vlastarakos PV, Andriopoulou E, Kreatsas G, Linos A. Factors affecting breast-feeding initiation in Greece: What is important? Midwifery. 2015; 31:323-331.
20. Sourila D, Alikari V, Prezerakos P, Tsironi M, Zyga S. Frequency of breastfeeding in postpartum women and related factors. Archives of Hellenic Medicine. 2015; 32:484-491.
21. Sencan I, Tekin O, Tatli MM. Factors influencing breastfeed¬ing duration: a sur56.vey in a Turkish population. Eur J Pediatr. 2013; 172:1459–1466.
22. Yılmaz E, Doğa Öcal F, Vural Yılmaz Z, Ceyhan M, Fadi Kara O, Küçüközkan T. Early initiation and exclusive breastfeeding: Factors influencing the attitudes of mothers who gave birth in a baby-friendly hospital. Turk J Obstet Gynecol. 2017; 14:1-9
23. Jaafar SH, Ho JJ, Lee KS. Rooming-in for new mother and infant versus separatecare for increasing the duration ofbreastfeeding. CochraneDatabaseof SystematicReviews 2016; 8: CD006641.
24. rgenekon-Ozelci P, Elmaci N, Ertem M, et al. Breastfeeding beliefs and practices among migrant mothers in slums of Diyarbakir, Turkey, 2001. Eur J Public Health. 2006; 16:143-8.
25. World Health Organization (WHO): Indicators for assessing infant and young child feeding practices Part 1 Definitions. Geneva: WHO; 2008.
26. Brystrova K, Widstrom AM, Matthiesen AS, et al. Early lactation performance in primiparous and multiparous women in relation to different maternity home practices. A randomised trial in St. Petersburg. International Breastfeeding Journal. 2007; 2:9.
27. Perez-Escamilla R, Segura-Millan S, Pollitt E, et al. Effect of the maternity ward system on the lactation success of low-income urban Mexican women. Early Human Development. 1992; 31:25-40.