Research
HJOG 2025, 24 (4), 242-255| doi: 10.33574/hjog.0605
Giannoula Kyrkou1, Artemis Koukoumbri1, Athina Diamanti1, Victoria Vivilaki1, Nikoleta Tsinisizeli1,2, Grigorios Karampas3, Anastasia Bothou1
1University of West Attica, School of Health and Care Sciences, Department of Midwifery, Athens, Greece
2General State Hospital of Nikaia “Agios Panteleimon”, Neonatal Intensive Care Unit, Athens, Greece
3Second Department of Obstetrics and Gynaecology, Aretaieio Hospital, National and Kapodistrian University of Athens, Athens, Greece
Correspondence: Giannoula Kyrkou, Telephone +030 210 538 7406, Ag. Spyridonos 28, Zip Code 12243, Athens, Greece, email: ikirkou@uniwa.gr
Abstract
Background: Human papillomavirus (HPV) is one of the most common sexually transmitted infections globally and is associated with the development of various malignancies, particularly cervical cancer. Given its public health impact, understanding the population’s knowledge, attitudes, and behaviors related to HPV is essential for the design of effective preventive strategies.
Aim: The aim of this study was to investigate the knowledge, beliefs, and behaviors of the population of Crete regarding HPV.
Methods: A descriptive cross-sectional study was conducted between November 2023 and January 2024. The questionnaire by Saulle et al. (2013) was used for data collection. Statistical analysis was performed using SPSS.
Results: Among the 130 participants, 40% reported obtaining information about HPV from a doctor, while 10% were unaware of the virus. Most respondents (72.3%) believed the state bears responsibility for public information. Regarding HPV vaccination, only 10% were vaccinated, while 33.3% cited older age as a reason for not receiving the vaccine. Moreover, 70% agreed that vaccination should occur before the onset of sexual activity. Half of the respondents reported engaging in sexual activity more than twice a week, while 20% had over five sexual partners in the last five years. Condom use was reported by only half of the participants. High awareness was observed regarding HPV’s association with cervical cancer (80.8%) and warts (83.8%), and 81.5% correctly stated that both men and women should be vaccinated.
Conclusions: The findings indicate a generally good level of knowledge about HPV among Cretan residents, particularly among those who received information from healthcare professionals. Structured, state-supported health education campaigns are needed to enhance public understanding and promote prevention efforts, including vaccination.
Keywords: HPV, vaccination, knowledge, attitudes, behaviors
Introduction
Human papillomavirus (HPV) is a DNA virus of the Papillomaviridae family and includes more than 200 identified genotypes, of which approximately 40 infect the anogenital mucosa and are transmitted primarily through sexual contact [1,2]. Based on oncogenic potential, HPV types are classified into low-risk types-typically associated with genital warts-and high-risk types, such as HPV-16 and HPV-18, which are strongly associated with the development of malignancies, particularly cervical cancer [3,4].
While the majority of HPV infections are asymptomatic and self-limiting, persistent infection with high-risk types can lead to precancerous lesions and invasive cancers affecting not only the cervix but also the anus, penis, oropharynx, and larynx [5,6]. HPV is now considered the most common sexually transmitted infection worldwide, posing significant challenges to public health systems due to both its silent progression and its oncogenic potential [7,8].
Global studies have revealed considerable variation in HPV prevalence by region. For instance, prevalence reaches as high as 57.7% in parts of Asia, 33.6% in East Africa, and around 20% in many European countries [8,9,10]. In Greece, studies have shown relatively high HPV prevalence rates as well, ranging from 22.7% to 24.6% among sexually active women [11,12,13].
HPV infection is most prevalent among young women under the age of 25 and is linked to risk factors such as early onset of sexual activity and a high number of sexual partners [14,15]. Prophylactic HPV vaccination, introduced over the past two decades, has demonstrated efficacy in preventing high-risk HPV infections and associated diseases [16]. Nevertheless, uptake rates remain suboptimal in many populations, often due to limited awareness, misinformation, and vaccine hesitancy [17,18].
Understanding the public’s knowledge, attitudes, and behaviors toward HPV is essential for the development of effective public health strategies. Despite the public health significance of HPV, no recent data exist on the level of awareness and behavioral patterns related to HPV in the Cretan population. This study aims to fill this gap by investigating the knowledge, perceptions, and preventive practices of individuals residing in Crete.
Aim
The aim of this study was to assess the knowledge, attitudes, and behaviors of adult residents of Crete regarding human papillomavirus (HPV) and its prevention.
Objectives
To evaluate the level of knowledge among participants about HPV transmission, associated diseases, and prevention strategies.
To assess attitudes toward HPV vaccination and the factors influencing vaccination uptake.
To investigate sexual behaviors and protective practices relevant to HPV transmission.
To explore the extent of engagement in cervical cancer screening (Pap test) among women.
To identify demographic and informational factors associated with HPV knowledge and preventive behavior.
Data collection
Data were collected using a structured questionnaire developed and previously validated by Saulle et al. (2013) for assessing knowledge, attitudes, and behaviors related to HPV in young women [19]. The original version of the instrument reported a Cronbach’s alpha of 0.78 in the validation study (Saulle et al., 2013). Given the scope and design of the current study, no additional reliability testing was conducted.
The questionnaire was translated into Greek and linguistically adapted for the target population following a forward–backward translation process. Although no formal psychometric validation (e.g., internal consistency analysis) was performed in the current study, the instrument was reviewed by a panel of health science professionals for face and content validity. A small pilot test (n=15) was also conducted to confirm the clarity and comprehension of the translated items.
The questionnaire consisted of three sections:
Section A: Demographics (age, gender, education, marital status, etc.)
Section B: Knowledge about HPV transmission, health implications, vaccination, and screening (14 items; score range: 0–14; scaled to 0–100).
Section C: Attitudes and self-reported behaviors regarding HPV vaccination, sexual health practices, and use of preventive services.
Materials and Methods
Study Design, Population & Setting: This study employed a descriptive cross-sectional design. Data were collected between November 2023 and January 2024 in the island region of Crete, Greece.
Crete is the largest island in Greece, with an estimated population of approximately 620,000 residents. It is characterized by a rich demographic and geographic diversity, combining urban centers, semi-urban areas, and rural communities. This diversity, along with the island’s cultural uniqueness, makes it a relevant and meaningful setting for examining public knowledge, attitudes, and behaviors related to HPV and its prevention.
The study targeted adult residents of Crete (aged ≥18 years), regardless of gender, educational background, or socioeconomic status. Participants were recruited using a convenience sampling method from public locations, healthcare facilities, and community settings across various regional units of the island.
Inclusion criteria included permanent residence in Crete, age 18 or older, ability to understand and complete the questionnaire in Greek, and provision of informed consent. Exclusion criteria included temporary residence, language or cognitive barriers, participation in another similar study, or refusal to participate voluntarily.
A total of 130 individuals participated in the study. No formal sample size calculation was conducted due to the exploratory nature of the research; however, efforts were made to include a demographically diverse sample.
Ethical Considerations: Participation was voluntary, anonymous and confidential, and although the study involved minimal risk, participants were informed of the purpose of the research and provided written consent.
Statistical Analysis
Data were entered and organized in Microsoft Excel and subsequently analyzed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY, USA).
Descriptive statistics were used to summarize the data. Categorical variables (e.g., gender, vaccination status, source of information) were presented as absolute and relative frequencies. Continuous variables (e.g., age, knowledge score) were summarized using means, standard deviations, and ranges where appropriate.
The primary outcome was the HPV knowledge score, derived from 14 multiple-choice items. Each correct answer was assigned 1 point; incorrect or “I don’t know” answers received 0 points. The raw score (range 0–14) was then normalized to a scale of 0 to 100 for interpretability.
Normality of the knowledge score distribution was assessed using Q-Q plots and the Shapiro-Wilk test. Due to substantial non-normality and skewness, non-parametric statistical tests were applied:
Mann–Whitney U test was used to compare knowledge scores between two independent groups (e.g., vaccinated vs. unvaccinated).
Kruskal–Wallis H test was used for comparisons among more than two groups (e.g., education levels).
Binomial tests were performed on individual knowledge items to assess whether the proportion of correct answers differed significantly from the expected 50% threshold.
All tests were two-tailed, and statistical significance was set at p < 0.05.
Results
Demographic Characteristics
A total of 130 individuals participated in the study, of whom 60.8% were women. The mean age was 39.7 years (SD ±12.2), with 52.3% of participants aged over 40. Most respondents had a university degree or higher (70.7%), while 64.6% were married or cohabiting (Table 1).
Knowledge About HPV
A high proportion of participants correctly identified the association between HPV and cervical cancer (80.8%) and genital warts (83.8%). However, knowledge was significantly lower regarding its association with other cancers, such as anal (32.3%), laryngeal (36.2%), and bladder (23.1%) cancer (Table 2).
Only 40% of participants reported having received information about HPV vaccination from a gynecologist, while 36.9% cited the internet as their main source. Notably, 9.2% stated they had no knowledge of the vaccine (Figure 1).
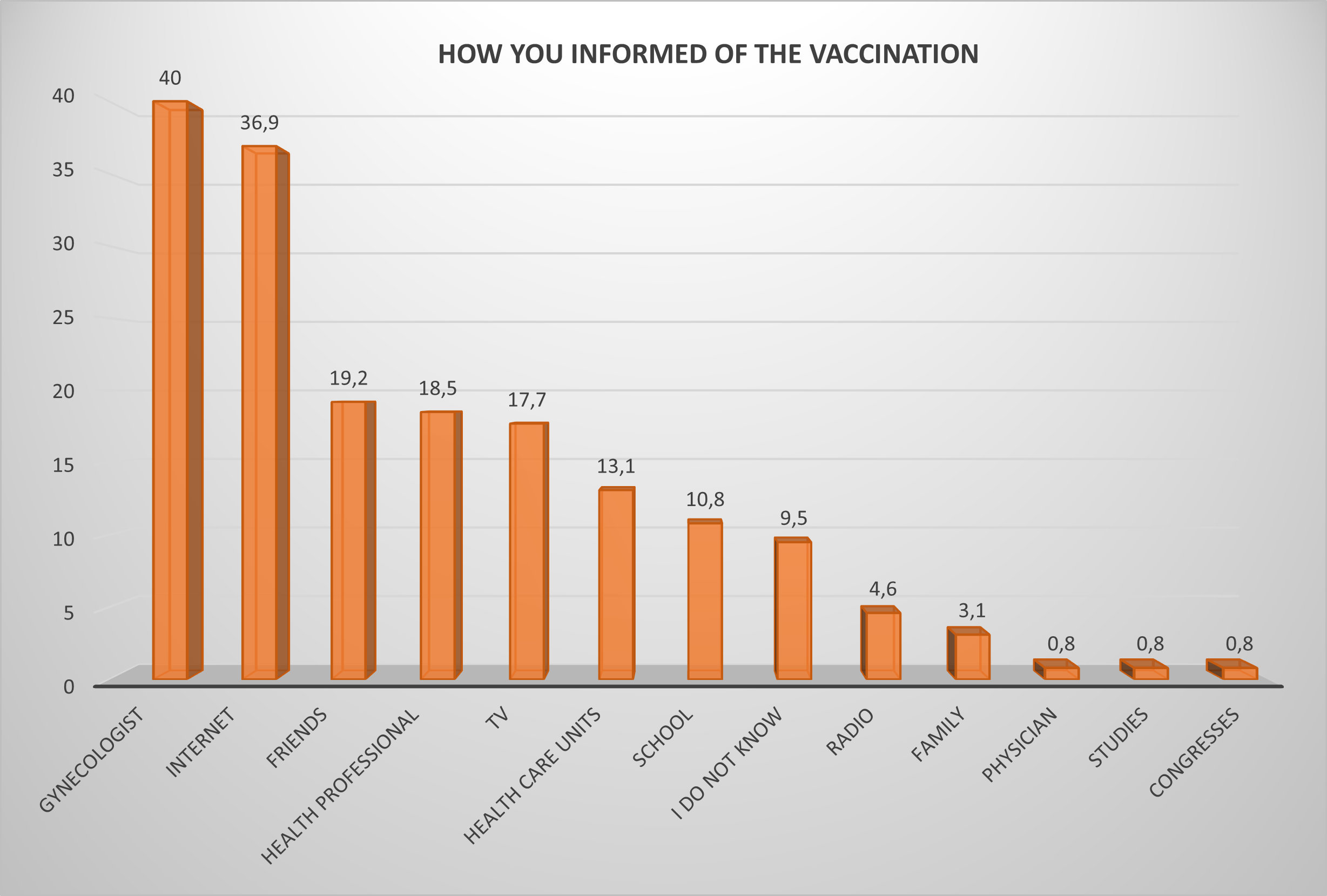
Figure 1. Sources of HPV vaccine information.
Vaccination Knowledge and Attitudes
Most participants (70%) correctly stated that HPV vaccination should occur before the onset of sexual activity. However, only 31% knew that the ideal age is 9–13 years, while 12% were unsure. A majority (81.5%) recognized that both men and women should be vaccinated (Figure 2).
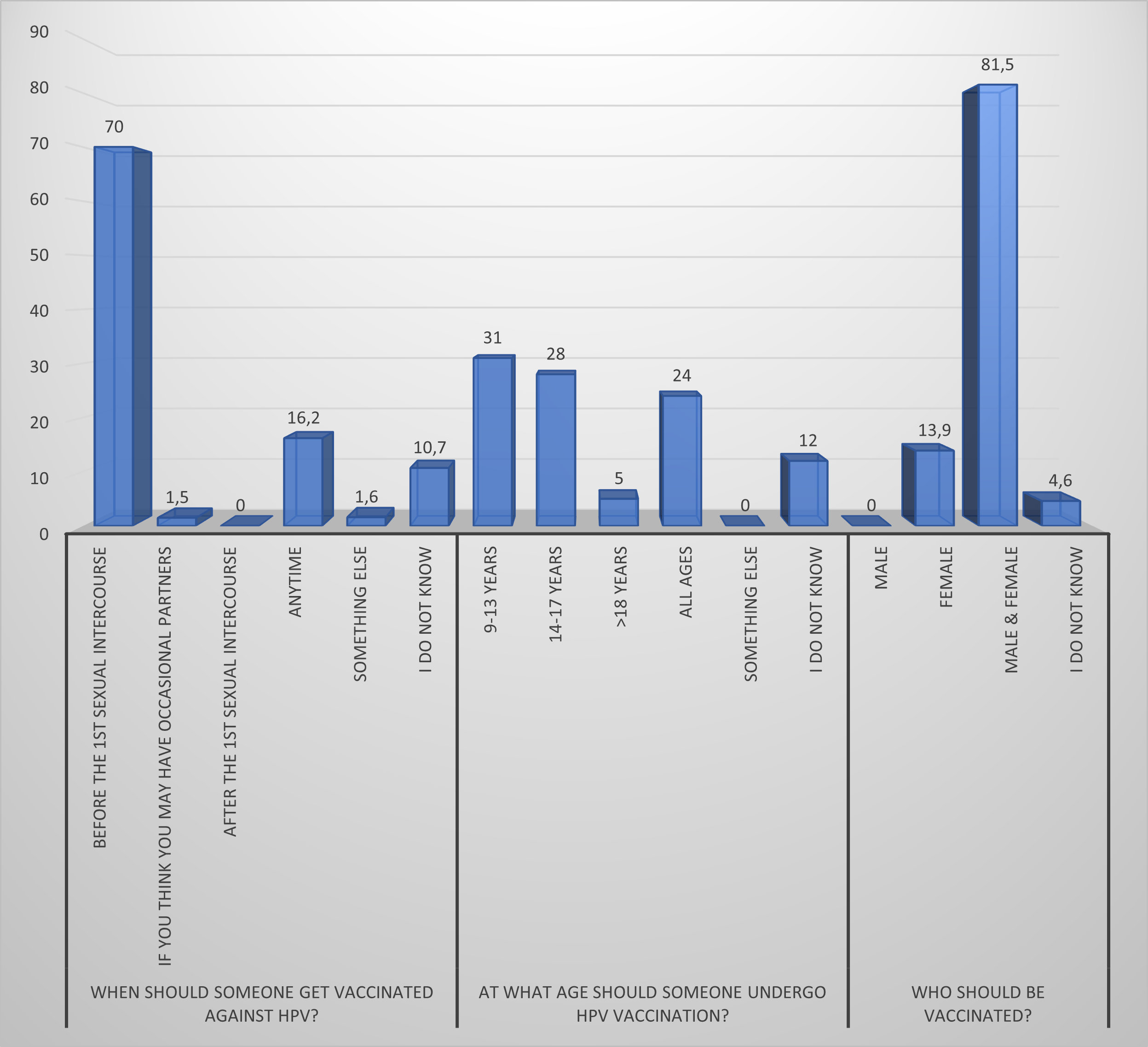
Figure 2. Vaccination knowledge.
Only 24.6% of respondents reported being vaccinated. The main reason for non-vaccination was “older age” (33.1%), followed by lack of medical advice (20.4%) and cost (11.2%) (Table 3) (Figure 3).
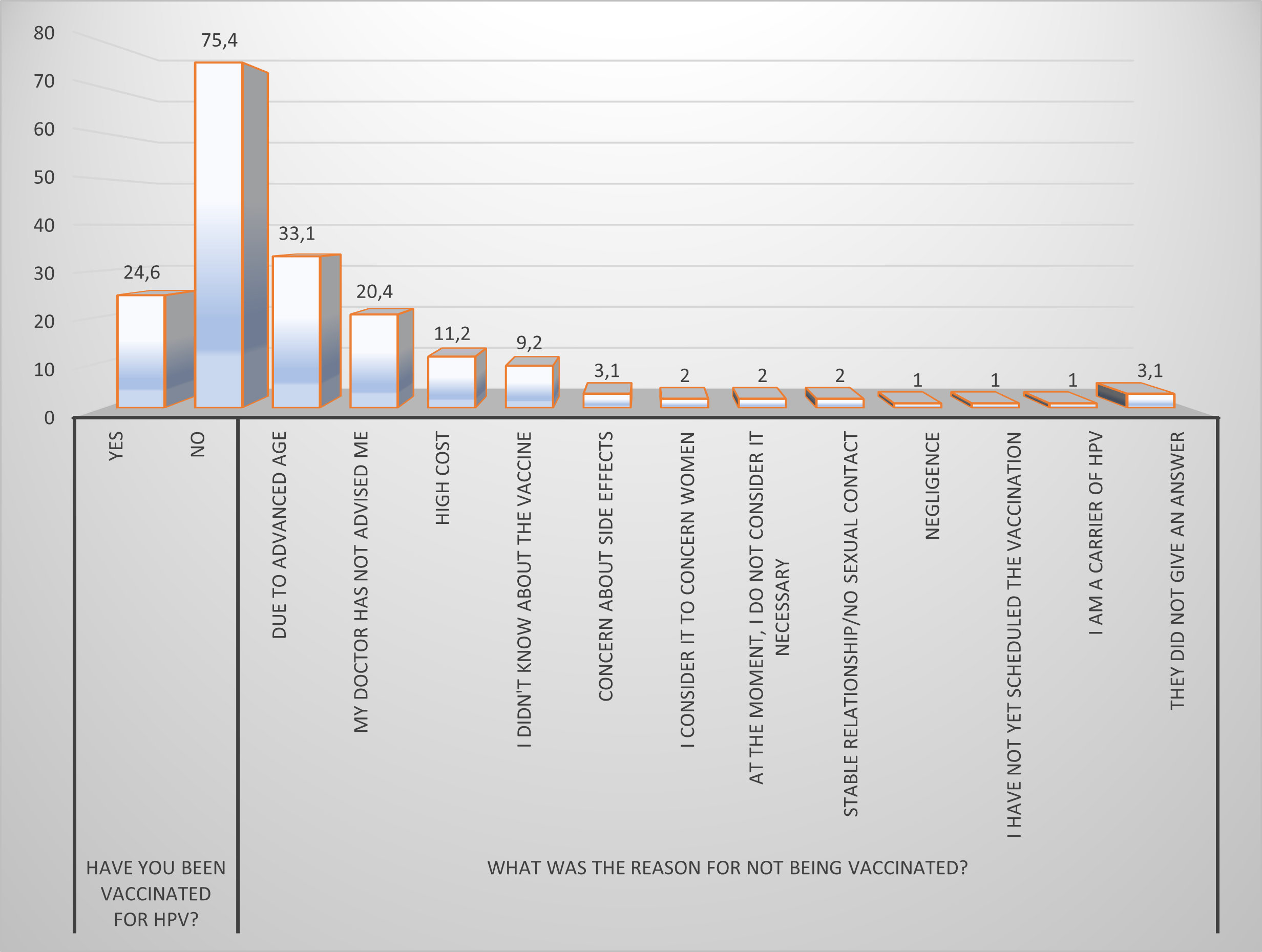
Figure 3. Vaccination status and reasons for non‐vaccination.
Sexual Behavior and Use of Protection
Half of the respondents (50%) reported having sexual intercourse more than twice per week. One in five (20.2%) reported having more than 5 sexual partners in the past 5 years. Despite this, condom use was inconsistent: 39.5% reported not using any contraceptive method, and 55.8% did not use a condom in their last sexual encounter (Table 4).
Pap Test and Preventive Practices
All female participants (100%) stated they were aware of the Pap test, and 93.7% had undergone one. All women reported satisfactory communication with their gynecologist. However, only 54.6% of all respondents had ever received information about HPV from a healthcare professional (Table 5).
HPV Knowledge Assessment
Participants’ responses to the structured knowledge assessment revealed strong awareness of HPV’s link to certain conditions. Specifically, 80.8% correctly associated HPV with cervical cancer and 83.8% with genital warts. In contrast, knowledge regarding other HPV-related diseases was considerably lower: only 36.2% identified a link with laryngeal cancer, 32.3% with anal cancer, and just 23.1% with either bladder or esophageal cancer. A notable 93.1% of respondents incorrectly denied any connection between HPV and irritable bowel syndrome, suggesting confusion about the virus’s scope.
In terms of transmission and symptomatology, a large majority (86.9%) erroneously believed that HPV infection is always symptomatic. Additionally, only 30.8% of participants correctly identified the appropriate vaccination age group (9–13 years), and just 40% reported having been informed about HPV vaccination by a gynecologist. On a more positive note, 81.5% of respondents accurately stated that both men and women should be vaccinated, reflecting encouraging levels of awareness regarding gender-inclusive prevention (Table 6).
These findings indicate a relatively high level of awareness regarding HPV’s primary risks but reveal persistent misconceptions related to transmission characteristics, disease range, and preventive guidelines.
Discussion
The findings of this study highlight both encouraging trends and critical gaps in the knowledge, attitudes, and behaviors of the adult population in Crete regarding HPV and its prevention. Participants demonstrated a relatively high level of awareness about the link between HPV and cervical cancer (80.8%) and genital warts (83.8%). These results are consistent with prior Greek studies, such as Georgiou (2023), in which 70.5% of women were aware of the connection between HPV and cervical cancer, and Paraskevopoulou (2021), where 93.3% of parents recognized this link [20,21). Similarly, in Litaina (2024), 90% of women reported awareness of the HPV vaccine [22].
However, knowledge of other HPV-related cancers as laryngeal, anal, bladder, remained limited in our study. Comparable findings were reported by Hatzi (2012) and Petroglou (2017), indicating that awareness continues to focus narrowly on cervical pathology [17,23]. This suggests that public health messaging in Greece has largely emphasized female reproductive consequences of HPV, potentially under-representing its broader oncogenic impact on both sexes.
National health education should broaden its scope to include HPV’s role in non-cervical cancers, especially oropharyngeal and anal cancers, with emphasis on relevance to both men and women.
A significant proportion of participants (86.9%) incorrectly believed that HPV infection always presents with symptoms. This reflects a misconception that may delay screening or preventive behaviors among asymptomatic carriers. In terms of vaccination awareness, although 70% of participants correctly indicated that the vaccine should be administered before sexual debut, only 31% correctly identified the recommended vaccination age (9–13 years). This finding mirrors the results of Peristeropoulou (2022), where just 12.9% answered this question correctly [24].
This discrepancy suggests a vague understanding of the timing of vaccination. It may reflect a lack of clear guidance from health professionals or a reluctance to discuss sexual health with preadolescents. Incorporating HPV education into school health programs, training pediatricians to recommend the vaccine at the appropriate age, and implementing appropriate policy strategies across the board could improve the gaps that exist.
Participants who had received information from a health professional demonstrated significantly higher knowledge scores (p < 0.05), a finding that supports previous literature [17,25]. However, only 40% of participants had been informed by a gynecologist or healthcare provider. This underlines the need to reinforce the role of health professionals in structured, standardized HPV counseling. This pattern, according to Gesouli-Voltyraki (2010) and Petroglou (2017), suggests a gap in regular preventive counseling [17,25]. Despite high participation of women in Pap smears, regular HPV counseling by health professionals appears limited. Structured provider-patient communication protocols should be developed, such as during Pap smear visits, with HPV counseling included as a standard part of reproductive care.
Regarding attitudes, 24.6% of respondents reported having been vaccinated, an uptake rate similar to that found in the study by Bosmi (2020), where nearly half of the parents had vaccinated their children [18]. Among the unvaccinated, the main reasons were older age (33.1%) and lack of medical recommendation (20.4%). The same barrier (inadequate doctor advice) was identified in Gesouli-Voltyraki (2010) and in the nursing student sample studied by Petroglou (2017), where students were aware of the vaccine but had not been guided toward vaccination [17,25]. This suggests that many adults mistakenly believe that they are not eligible for vaccination or that the window for effectiveness has passed. Adults with ongoing sexual activity remain vulnerable and may not perceive the benefit of even delayed vaccination. Public health authorities should clarify that HPV vaccination remains effective even after the onset of sexual activity and, in many countries, is recommended up to the age of 45, based on shared decision-making.
Regarding sexual habits, half of the participants in this study reported having sex more than 2 times a week, while 20% of the participants stated that in the last 5 years they had had more than 5 sexual partners, while only half of them use condoms as a means of protection. Similar findings were found in the study by Peristeropoulou (2022) [24], 61.7% of the participants stated that they are sexually active, 47.1% stated that they have 2-5 sexual partners, and 68% stated that they always or almost always use condoms. Similarly, in the study by Georgiou (2023) [20], 58.4% of the respondents stated that condoms are a preventive measure for them. This indicates a discordance between knowledge and preventive behavior, possibly linked to perceptions of monogamy, trust, or reduced concern about HPV among older adults. Tailored health promotion campaigns, particularly via social media or peer-education methods, should target sexually active adults with messages reinforcing condom use and routine screening.
On a more positive note, Pap test awareness and uptake were remarkably high: all women in this study knew about the test and 93.7% had undergone it, with good communication with their gynecologist. This is a significant improvement compared to older findings: in Georgiou (2023), only 67.6% recognized the importance of regular screening, and in Litaina (2024), 79.9% reported participating in cervical screening programs [20,22]. The well-established acceptance of cervical screening could be strategically employed as a vehicle for disseminating HPV-related education, with a particular focus on reaching unvaccinated or older female populations.
Overall, this study confirms that although basic knowledge about HPV is improving over time in Greece, there remain important gaps and misconceptions, especially regarding transmission, vaccine eligibility, and the virus’s broader disease spectrum. Targeted, structured interventions by the healthcare system are urgently needed to transform knowledge into action and ensure consistent preventive behavior across the lifespan.
Strengths & Limitations
This is a study that assesses knowledge, attitudes, and behaviors related to HPV in the general adult population of Crete, providing new data from a geographically and culturally distinct region of Greece. The study used a previously validated questionnaire (Saulle et al., 2013), which was linguistically and culturally adapted for the Greek population, ensuring conceptual equivalence and content validity. The sample included a wide range of participants, both in terms of age and educational level, enhancing the representativeness of the findings in the context of the island. The study covered a wide range of topics – knowledge, attitudes, vaccination, sexual behaviors, and sources of information – providing a comprehensive picture of public awareness and practices related to HPV.
The use of a convenience sampling method may have introduced selection bias, as individuals who were more health-conscious or health-engaged may have been more likely to participate. Due to the cross-sectional design, causality cannot be inferred. Observed associations reflect association, not directionality. The sample size, although sufficient for descriptive analysis, was relatively small (n = 130), limiting generalizability and reducing statistical power for subgroup comparisons. The data were self-reported by participants, which may have introduced recall or social desirability bias, especially regarding sensitive questions related to sexual behavior and vaccination status.
Conclusions
This study provides important insight into the current state of public knowledge, attitudes, and behaviors regarding HPV among adult residents of Crete. While awareness of HPV’s link to cervical cancer and the existence of the Pap test was high, considerable knowledge gaps were identified, particularly concerning the asymptomatic nature of HPV, the recommended age for vaccination, and its association with non-cervical cancers.
Participants who had received information from healthcare professionals exhibited significantly higher knowledge levels, underscoring the critical role of provider-led education. However, low overall vaccination coverage and inconsistent use of protective behaviors suggest that knowledge alone is insufficient to ensure action.
Strengthening structured HPV-related communication within primary care and gynecological settings, promoting early adolescent vaccination through school-based programs, and addressing misconceptions through targeted health campaigns are essential next steps. Public health strategies should be tailored to include both men and women, and extend beyond reproductive age groups to capture at-risk adults who remain unvaccinated.
In conclusion, while progress has been made in raising HPV awareness, coordinated, evidence-based interventions are required to translate knowledge into sustained preventive behaviors and to improve vaccination uptake in the general population.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
Data Availability Statement
All data generated or analysed during this study are included in this published article.
Funding
No funding was received for this study.
References
- Anderson S, Safari H, Mints M, et al. Type distribution, viral load and integration status of high-risk human papillomaviruses in pre-stages of cervical cancer (CIN). British Journal of Cancer. 2005;92(12):2195-2200. doi.10.1038/sj.bjc. 6602648
- Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370(9590):890-907. doi.10.1016/s0140-6736(07) 61416-0
- Doorbar J, Quint W, Banks L, et al. The biology and life-cycle of human papillomaviruses. Vaccine. 2012;30:F55-F70. doi.10.1016/j.vaccine. 2012.06.083
- Schiffman M, Doorbar J, Wentzensen N, et al. Carcinogenic human papillomavirus infection. Nature Reviews Disease Primers. 2016;2: 16086. doi. 10.1038/nrdp.2016.86
- Syrjänen S. Human papillomavirus infections and oral tumors. Medical Microbiology and Immunology. 2003;192(3):123-128. doi. 10.1007/ s00430-002-0173-7
- Martino M, Haitel A, Wrba F, et al. High-risk human papillomavirus infection of the foreskin in asymptomatic boys. Urology. 2013;81 (4):869-872.doi.10.1016/j.urology. 2012.12.011
- Harari A, Che Z, Burk RD. HPV genomics: past, present and future. Current Problems in Dermatology. 2014;45:1-18. doi. 10.1159/000355952
- De Sanjosé S, Diaz M, Castellsagué X, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. The Lancet Infectious Diseases. 2007;7(7):453-459. doi. 10.1016/s1473-3099(07)70158-5
- Arbyn M, Anttila A, Jordan J, et al. European guidelines for quality assurance in cervical cancer screening. Second edition–summary document. Annals of Oncology. 2010;21(3):448-458. doi. 10.1093/annonc/mdp471
- Muñoz N, Manalastas R Jr, Pitisuttithum P, et al. Safety, immunogenicity, and efficacy of quadrivalent human papillomavirus (types 6, 11, 16, 18) recombinant vaccine in women aged 24-45 years: a randomised, double-blind trial. Lancet. 2009;373(9679):1949-1957. doi. 10.1016/s01 40-6736(09)60691-7
- Kroupis C, Thomopoulou G, Papathomas TG, et al. Population-based study of human papillomavirus infection and cervical neoplasia in Athens, Greece. Epidemiology and Infection. 2007;135:943-950. doi. 10.1017/s095026880700876x
- Panotopoulou E, Tserkezoglou A, Kouvousi M, et al. Prevalence of human papillomavirus types 6, 11, 16, 18, 31, and 33 in a cohort of Greek women. Journal of Medical Virology. 2007;79:1898-1905. doi. 10.1002/jmv.21025
- Stamataki P, Papazafiropoulou A, Elefsiniotis I, et al. Prevalence of HPV infection among Greek women attending a gynecological outpatient clinic. BMC Infectious Diseases. 2010;10:27. doi. 10.1186/1471-2334-10-27
- Thanasas IK, Lavranos G, Gogkou P, et al. Epidemiology of HPV in Greece and other countries of the world. Scientific Chronicles. 2020;25(1):132-147. http://www.tzaneio.gr/wp-content/uploads/epistimonika_xronika/p20-1-9.pdf
- Bruni L, Albero G, Rowley J, et al. Global and regional estimates of genital human papillomavirus prevalence among men: a systematic review and meta-analysis. The Lancet Global Health. 2023; 11:e1345-e1362. doi. 10.1016/s2214-109x(23) 00305-4
- Castle PE, Maza M. Prophylactic HPV vaccination: past, present and future. Epidemiology and Infection. 2016;144(3):449-468. doi. 10.1017/s0950268815002198
- Petroglou S, Fotos N, Brokalaki H. Knowledge, attitude and behavior of nursing students towards HPV. Hellenic Journal of Nursing. 2017; 56 (2): 149 – 156.
- Bosmi I. Parents’ views on the vaccination of 5th and 6th grade children against human papillomavirus in primary schools of the municipality of Pefki. [Thesis] Larissa: University of Thessaly. 2020. doi. 10.26253/heal.uth. 8466
- Saulle R, Miccoli S, Unim B, et al. Validation of a questionnaire for young women to assess knowledge, attitudes and behaviors towards cervical screening and vaccination against HPV in Italy. Epidemiology Biostatistics and Public Health. 2024;11(2):e8913. doi. 10.2427/ 8913
- Georgiou E. Women’s knowledge and attitudes towards the ΗPV vaccine. [Thesis] Athens: University of West Attica. 2023. https://polynoe.lib.uniwa.gr/xmlui/bitstream/handle/11400/5108/Georgiou_20014.pdf.pdf?sequence=1&isAllowed=y
- Paraskovopoulou C. Parents’ knowledge, perceptions and attitudes on vaccination of boys against Human Papilloma Virus (Hpv). [Thesis] Tripoli: University of Peloponnese. 2021. https://amitos.library.uop.gr/xmlui/bitstream/handle/123456789/6379/%ce%94%ce%99%ce%a0%ce%9b%ce%a9%ce%9c%ce%91%ce%a4%ce%99%ce%9a%ce%97%20%ce%95%ce%a1%ce%93%ce%91%ce%a3%ce%99%ce%91%20%ce%a0%ce%91%ce%a1%ce%91%ce%a3%ce%9a%ce%95%ce%a5%ce%9f%ce%a0%ce%9f%ce%a5%ce%9b%ce%9f%ce%a5%20%ce%a7%ce%a1%ce%a5%ce%a3%ce%9f%ce%a5%ce%9b%ce%91%20%281%29.pdf?sequence=3&isAllowed=y
- Litaina Th. Women’s knowledge and perceptions regarding human papillomavirus (HPV) and cervical cancer prevention. [Thesis] Larissa: Hellenic Open University. 2024. https://apothesis.eap.gr/archive/item/198605?lang=el
- Hatzi P. Knowledge, attitudes and opinions of female health professionals on HPV prevention. [Thesis] Larissa: University of Thessaly. 2012. doi. 10.26253/heal.uth.4348
- Peristeropoulou P. Investigation of knowledge, attitudes and practices regarding HPV among students of the University of Patras. [Thesis] Patras: Hellenic Open University. 2022. https://apothesis.eap.gr/archive/item/170893
- Gesouli – Voltyraki E, Kanavou V, Ifantis A, et al. Investigation of knowledge and practices regarding the Papanicolaou test, among female health professionals. The Step of Asklepios. 2010; 9 (1): 100 – 114. https://www.vima-asklipiou.gr/images/upload/various/files/8585829362539475521Tc7bdCk3F4eV4qBYMpod8585756244119737692.pdf